Seguridad del paciente
WHEC Boletín Práctica Clínica y Gestión de los proveedores de salud. Educación subvención prevista de Salud de la Mujer y el Centro de Educación (WHEC).
Patient safety is a fundamental principle of health care. Progress in patient safety has been exceedingly slow, hampered by lack of both clarity regarding the definition and standard methodology to assess iatrogenic patient harm in obstetrics and gynecology. Understanding the causes of medical error and strategies to reduce harm is simple compared with the complexity of clinical practice. On the other hand, patient safety interventions will not be successful without a receptive culture of safety. This culture can only occur with engaged organizational and individual leaders who understand the importance of patient safety. Twenty years ago, whenever discussion about patient safety came-up, the most common question from medical professionals was "What is patient safety?" Now, with a growing sense of urgency to reduce iatrogenic harm, the most common question is "How can I reduce medical errors and improve patient safety?" Communication breakdown remains a leading contributor to adverse events in the United States (1). Every point in the process of care-giving contains a certain degree of inherent unsafety. A number of countries have published studies showing that significant numbers of patients are harmed during health care, either resulting in permanent injury, increased length of stay in health care facilities, or even death. Clear policies, organizational leadership capacity, data to drive safety improvements, skilled health care professionals and effective involvement of patients in their care, are all needed to ensure sustainable and significant improvements in the safety of health care. Apart from the human cost, medication errors place an enormous and unnecessary strain on health budgets. Preventing errors saves money and saves lives. Every person around the world, at some point in their life, will take medicines to prevent or treat illness. However, medicines do sometimes cause serious harm if taken incorrectly, monitored insufficiently or as the result of an error, accident or communication problems.
The purpose of this document is to discuss strategic pathways to accelerate future improvement in patient safety. It includes fundamental changes in health care education, patient engagement, transparency, care coordination, and improving health care providers' morale. Transforming groups of individual experts into expert teams is central to this cultural transformation. This document aims to address the weakness in health systems that lead to medication errors and severe harm that results. It lays out ways to improve the way medicines are prescribed, distributed, and increase awareness among patients about the risks associated with the improper use of medications. Both health workers and patients can make mistakes that result in severe harm, such as prescribing, ordering, dispensing, preparing, administrating or consuming the wrong medication or the wrong dose at the wrong time. But all medication errors are potentially avoidable. Preventing errors and the harm that results requires putting systems and procedures in place to ensure the right patient receives the right medication at the right dose at the right time.
Introduction
Patient safety is a global public health issue, causing death and suffering in all types of patients and incurring costs in all countries. The global health community has made significant and sustained efforts to improve safety and quality of health services. Medication errors cause at least one death every day and injure approximately 1.3 million people annually in the United States of America (USA) alone (2). While low- and middle-income countries are estimated to have similar rates of medication-related adverse events to high-income countries, the impact is about twice as much in terms of number of years of healthy life lost. Many countries lack good data, which will be gathered as part of this initiative. Globally, the cost associated with medication errors has been estimated at US$ 42 billion annually or almost 1% of total global health expenditure (2). Mediation errors can be caused by health worker fatigue, overcrowding, staff shortages, poor training and the wrong information being given to patients, among other reasons. Any one of these, or a combination, can affect the prescribing, dispensing, consumption, and monitoring of medications, which can result in severe harm, disability and even death.
A sentinel event is a Patient Safety Event that results in any of the following to a patient:
- Death;
- Permanent harm;
- Severe temporary harm and intervention required to sustain life.
Such events are called "sentinel" because they signal the need for immediate investigation and response. Self-reporting gives the opportunity to collaborate with a patient safety experts, reporting raises the level of transparency in the organization and promotes a culture of safety, and reporting conveys the health care organization's message to the public that it is doing everything possible, proactively, to prevent similar patient safety events in the future. Further, reporting the event enables "lessons learned" from the event to be added to joint efforts of The Women's Health and Education Center (WHEC) with the World Health Organization (WHO), thereby contributing to the general knowledge about sentinel events and to the education to the reduction of risk for such events.
Definitions
What is patient safety? Although much work has been done in the field, there is still no universally accepted definition of patient safety. Is patient safety a philosophy, a way of doing things, a discipline, or an attribute of care delivery systems? How does it differ from quality improvement? Acknowledging that patient safety is both a way of doing things and an emergent discipline, a definition for patient safety has emerged from the health care quality movement that is equally abstract, with various approaches to the more concrete essential components. Patient safety was defined by the Institute of Medicine as "the prevention of harm to patients" (3). Emphasis is placed on the system of care delivery that:
- Prevents errors;
- Learns from the errors that do occur; and
- It is built on a culture of safety that involves health care professionals, organization, and patients. The glossary at the Agency for Healthcare Research and Quality (AHRQ) Patient Safety Network expands upon the definition of prevention of harm: "freedom from accidental or preventable injuries produced by medical care" (4).
Patient safety practices have been defined as "those that reduce the risk of adverse events related to exposure to medical care across a range of diagnoses or conditions" (2),(4). This definition is concrete but quite incomplete, because so many practices have not been well studied with respect to their effectiveness in preventing or ameliorating harm. Practices considered to have sufficient evidence to include in the category of patient safety practices are as follows:
- Appropriate use of prophylaxis to prevent venous thromboembolism in patients at risk;
- Use of perioperative beta-blockers in appropriate patients to prevent perioperative morbidity and mortality;
- Use of maximum sterile barriers while placing central intravenous catheters to prevent infections;
- Appropriate use of antibiotics prophylaxis in surgical patients to prevent post-operative infections;
- Asking that patients recall and restate what they have been told during the informed-consent process to verify their understanding;
- Continuous aspiration of subglottic secretions to prevent ventilator-associated pneumonia;
- Use of pressure-relieving bedding materials to prevent pressure ulcers;
- Use of real-time ultrasound guidance during central line insertion to prevent complications;
- Patient self-management for warfarin (Coumadin ®) to achieve appropriate outpatient anticoagulation and prevent complications;
- Appropriate provision of nutrition, with a particular emphasis on early enteral nutrition in critically ill and surgical patients, to prevent complications;
- Use of antibiotic-impregnated central venous catheters to prevent catheter-related infections.
The World Health Organization (WHO), at the launch of their Alliance for Patient Safety in October 2004, defined patient safety and also the discipline of patient safety as: "Patient safety is the absence of preventable harm to a patient during the process of health care. The discipline of patient safety is the coordinated effort to prevent harm, caused by the process of health care itself, from occurring to patients" (5). The National Patient Safety Foundation, the largest multidisciplinary organization in USA devoted solely to the reduction of harm from medical error, defined patient safety as: "The avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the processes of health care including errors, deviations and accidents. Safety emerges from the proper interaction of the components of the health care system" (6). Finally, implicit in all these definitions is the understanding that, because of the complexity of health care, some errors are unavoidable. Therefore, the discipline of patient safety should first strive to reduce the number of errors, but most important, when errors do occur, medical systems should also have "safety nets" to prevent errors from causing patient harm.
The Venn diagram (see below, figure 1) is helpful in understanding some key patient safety concepts in relation to medical errors (7). An adverse event is an injury caused by medical management, not the underlying illness. Preventable adverse event is an adverse event caused by error and error is failure of a planned action to be completed as intended or use of a wrong plan to achieve an aim. Near misses are an important subset of medical errors. Analysis of near misses can help us redesign the medical system to prevent errors from causing patient harm by improving the resiliency of defensive barriers.
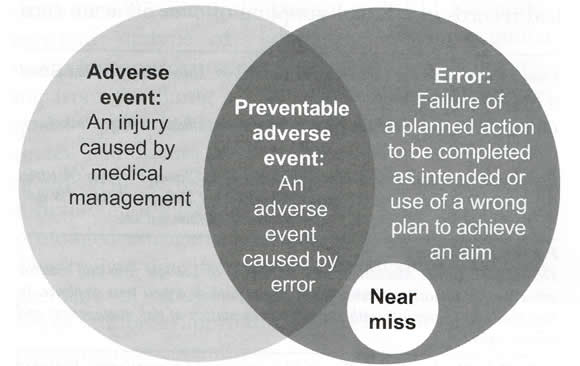
Once an error occurs, it may be (a) inconsequential; (b) cause patient harm; and (c) have the potential to cause harm until something else intervenes to prevent patient injury. The latter is known as a near miss.
What Causes Medical Errors?
Understanding why preventable adverse events occur will lead to strategies to reduce their incidence. Four factors in health care contribute to preventable adverse events:
- Human fallibility;
- Complexity;
- System deficiencies; and
- Vulnerability of defensive barriers.
Patient safety will only improve by first reducing the number of errors that occur, and second, preventing those errors that occur from harming patients (8).
Human Fallibility: To err is human. Being fallible is an unavoidable part of the human condition. In general, health care providers are among the most highly trained and dedicated individuals in society. They try their best every day with every patient but work in a flawed system. The solution to this problem must be to redesign the system, making it easy to do the right thing and hard to do the wrong thing and not to demand perfection in human performance.
Complexity: Modern health care is one of the most complex activities undertaken by human beings. The more complex the process, the less likely it can be executed without error. Simply by reducing the number of steps and the complexity in any given process, we can significantly reduce error and improve safety.
System Deficiencies: Modern health care is one of the most complex activities undertaken by human beings. The more complex the process, the less likely it can be executed without error. Simply by reducing the number of steps and the complexity in any given process, we can significantly reduce error and improve safety.
Vulnerability of Defensive Barriers: Defensive barriers are countermeasures designed to prevent errors from causing patient harm. Even the most robust countermeasures have inherent vulnerabilities. The more prevalent the gaps, the greater probability that errors will lead to patient harm. For example, miscommunication is one of the most common causes of error, especially in perinatal care. Several tools can be used to make communication clear. One example is closed loop communication which the recipient of a message repeats it back to the sender to be sure it is heard correctly.
CULTURE OF SAFETY: The Critical Role of Leadership
The critical role of effective leadership, not only in establishing a culture of safety, but also in improving outcomes, is evident in health care as well as other high-risk, complex fields such as aviation (9). Conversely, deficient leadership was identified as a contributing factor in 50% of the sentinel events reported to The Joint Commission in 2006. The Joint Commission's Sentinel Event Database reveals that leadership's failure to create an effective safety culture is a contributing factor to many types of adverse events - from wrong site surgery to delays in treatment (10). Leaders can build safety cultures by readily and willingly participating with care team members in initiatives designed to develop and emulate safety culture characteristics. Effective leaders who deliberately engage in strategies and tactics to strengthen their organization's safety culture see safety issues as problems with organizational systems, not their employees, and see adverse and close calls ("near misses") as providing "information-rich" data for learning and systems improvements. Individuals within the organization respect and are wary of operational hazards, have a collective mindfulness that people and equipment will sometimes fail, defer to expertise rather than hierarchy in decision-making, and develop defenses and contingency plans to cope with failures. These concepts stem from the extensive research of James Reason on psychology of human error. Among Reason's description of the main elements of safety culture are (11):
- Just culture - people are encouraged, even rewarded, for providing essential safety-related information, but clear lines are drawn between human error and at-risk or reckless behaviors;
- Reporting culture - people report their errors and near-misses;
- Learning culture - the willingness and the competence to draw the right conclusions from safety information systems, and the will to implement major reforms when their need is indicated.
Although it is clear that safety in health care is rooted on the essential components of that culture. It is important to sustain a culture of safety and commitment to safety at the highest levels of the organization and necessary resources for safety are provided making safety the highest priority. All workers must communicate effectively about safety concerns and there is transparency in reporting errors. Safety solutions should focus on system improvement, not individual blame and hazardous acts are rare. Willful violations and disruptive behaviors cannot be tolerated by leaders and they must respond with escalating levels of discipline.
Leadership Tools to Establish a Patient Safety Culture
An obstetrician-gynecologist may be faced with a sudden patient emergency at any time. Whether it is severe shoulder dystocia, catastrophic surgical or obstetric hemorrhage, or an anaphylactic reaction to an injection in the office. It will require prompt response. Over the decade, severe maternal morbidity in the United States has increased by 75% for complications associated with delivery, and specifically 114% for postpartum hemorrhage (12). Preparation for potential emergencies requires planning and interdisciplinary collaboration. Issues to consider include advance provisioning of resources, establishing and early warning system, designating specialized first responders, and holding drills to ensure that everyone knows what to do (13). Excellent communication and teamwork will further increase the efficiency and effectiveness of the emergency response.
Examples of Tools for Managing Clinical Emergencies:
- Availability of appropriate emergency supplies in a resuscitation cart (crash cart) or kit;
- Development of a rapid response team;
- Development of protocols that include clinical triggers;
- Use of standardized communication tools for huddles and briefs (e.g. Situation-Background-Assessment-Recommendation [SBAR]);
- Implementation of emergency drills and simulations.
RAPID RESPONSE TEAM
Rapid response team comprise of a diverse range of clinicians and stakeholders who bring critical care expertise to the patient's bedside or wherever it is needed. Rapid response team may include advanced practice nurses, respiratory therapists, and first responders who approach the scenario in a standardized fashion. The activation of a rapid response team should be simultaneous with the event. All regular clinical team members have the authority to activate a rapid response team when a critical situations are noted, or for any potential of serious emergency in which a team response is required (14). By designating criteria that define an emergency, it becomes clear when to call for help, thus increasing the utilization of the rapid response team. Early activation of a rapid response team has been associated with a decrease in cardiac arrest, improved survival of hospitalized patients, and decreased admissions to an intensive care unit. It is important to emphasize that calling a resident physician in a teaching hospital is not a substitute for triggering a rapid response team intervention. Similarly, calling the in-house physician in a non-teaching setting does not substitute activating a rapid response team intervention.
Establishing a rapid response team is a multistep process. Clinicians, support staff, and stakeholders must be identified. This may include the page operator, as well as staff in the blood bank or hospital laboratory. Criteria for activation of a rapid response team should be documented. A protocol that designates each team member's role must be implemented with drills and ongoing training. Debriefing, with feedback and process improvement, must be established. Finally, the effectiveness of the rapid response team process should be evaluated on a regular basis. A rapid response team can be divided into four components (15):
- Activators; these are individuals who may activate the rapid response team, and may include clinicians, specialists, or clerical staff. Team members from the nursing staff or floor staff are trained to monitor for disturbances that require activation to the rapid response team.
- Responders; these are clinicians who arrive at the bedside, along with the attending physician, to stabilize the patient and determine the patient's disposition. When the responders arrive, the activators must be prepared to exchange information. A communication protocol such as SBAR allows team members to exchange information in a clear and concise manner. The primary purpose of the communication protocol is to exchange critical patient information and establish treatment plan.
- Quality improvement; team members should be debriefed after the event in an effort to evaluate and improve their response. The quality improvement team reviews the activation, implementation, and outcomes of the rapid response team. Their assessment and recommendations are formulated into an action review, which may be implemented by administration.
- Administration; development of a rapid response team is a patient safety initiative promoted by the Women's Health and Education Center (WHEC) in collaboration with its partners. Successful implementation of a rapid response team may involve overcoming logistic, political, institutional, social, financial, or anthropologic barriers. Leadership for senior medical and nursing personnel is crucial (16).
EMERGENCY DRILLS AND SIMULATIONS
The principle that standardized care can result in safer care applies to emergency situations as well as to routine care. Periodic drills that follow a designated protocol for the management of common emergencies, such as fetal bradycardia or postpartum hemorrhage, may improve a health care unit's ability to respond to and mitigate and adverse outcome. The training may use a comprehensive curriculum that addresses communication strategies such as TeamSTEPPS (17) or a less structured teamwork model or a curriculum that focuses on specific clinical scenarios, such as shoulder dystocia. A sophisticated simulated environment or an everyday workspace can meet the needs of the trainees as long as it mirrors the existing clinical setting and resources. By conducting a drill in the actual patient care setting, issues related to the physical environment may become obvious. Simulation training can identify and correct common clinical errors made during emergencies. Protocols, activation criteria, and critical interventions can be reinforced by being posted on the walls, printed on pocket cards, or uploaded as screen savers to promote a sustained culture of safety.
Emergency drills allow team members to practice effective communication in a crisis. Adult learning theory supports the importance of experimental learning. Many aspects of the medical environment may compromise effective communication, including a hierarchical hospital structure, emotional intensity and stress of a situation, and the range of educational backgrounds and clinical understanding of various team members. Other barriers to improved response to medical emergencies include inadequate leadership, adherence to traditional models, fear of criticism, hierarchy and intimidation, failure to function as a team, and lack of education and orientation of involved staff (18).
Effective teamwork requires a team leader to coordinate the response, but it also empowers all members of the team to contribute and share information. By practicing together, barriers that hinder communication and teamwork can be overcome. Effective drills may lead to improved standardization of response, health care provider satisfaction, and patient outcomes. Developing rapid response team and training using drills and simulations may allow for faster and improved response to emergent situations, thereby potentially maximizing patient outcomes.
Implementation of Risk-Based Thromboembolism Prevention
Thromboembolism is one of the leading causes of maternal deaths in developed countries accounting for approximately 15% of maternal deaths (19). In United Kingdom, the publication of a Royal College of Obstetricians and Gynecologists (RCOG) Green-top Guideline with recommendations for risk-based low-molecular-weight heparin prophylaxis coincided with a reduction in maternal deaths from 1.94 deaths per 100,000 live births to 0.79 deaths per 100,000 live births (20). Recently, in the United States, the National Partnership for Maternal Safety released a bundle for thromboembolism prevention advocating for universal risk assessment and development of a prophylaxis protocol that fits each institution's needs and resources. Protocols and guidelines for thromboembolism prophylaxis are now commonplace for most medical and surgical admissions. However, there is concern within the obstetric community about application of these risk scoring systems from other specialties to otherwise young and healthy postpartum women given the low incidence of thromboembolism and unproven benefit in this population.
In this study (21), a risk-based protocol modified from RCOG guidelines was developed and initiated through health care provider education and protocol algorithms that were posted at health care provider workstations. Implementation of a low-molecular-weight heparin risk-based protocol for postpartum thromboembolism prevention resulted in high physician adherence and more than 30% of postpartum women receiving enoxaparin (21).
Algorithm for implementation of risk-based low-molecular-weight heparin venous thromboembolism prevention protocol in postpartum women
Thromboembolism risk-factors:
- Smoker;
- Parity >3;
- Age >35 years;
- Body Mass Index (BMI) >30 kg/m2 www.womenshealthsection.com/content/obs/bodymassindex.php3 or www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmi-m.htm
- Preeclampsia;
- Pregnancy from Assisted Reproductive Technology (ART);
- Varicose veins;
- Operative procedures;
- Multiple gestation;
- Blood transfusion;
- Current systemic infection;
- Dehydration or hyperemesis;
- Medical comorbidities;
- Long-distance travel (>4 hours);
- Immobility (e.g. bedrest);
- Prolonged labor in hospital (>24 hours).
Risk Factor Category and Recommendations:
- <3 risk-factors; sequential compression device (SCDs) and early ambulation.
- 3 risk-factors or BMI >40 kg/m2:
- If BMI is <40 kg/m2 enoxaparin 40 mg daily for 7 days prophylaxis, and
- If BMI is >40 kg/m2 enoxaparin 40 mg twice daily for 7 days prophylaxis.
- >4 risk-factors;
- If BMI <40 kg/m2 enoxaparin 40 mg daily for 6 weeks prophylaxis, and
- If BMI >40 kg/m2 enoxaparin 40 mg twice daily for 6 weeks prophylaxis.
MATERNAL SAFETY: Severe Hypertension during Pregnancy and Postpartum Period
Complications arising from hypertensive disorders of pregnancy are among the leading causes of severe maternal morbidity and preventable maternal mortality. Hypertensive-related complications can be significantly reduced through timely and appropriate treatment. To accelerate implementation of a comprehensive approach to a hypertensive crisis, a multidisciplinary work-group of the National Partnership for Maternal Safety, within the Council on Patient Safety in Women's Health Care, has developed a bundle for management of hypertensive crises during pregnancy and the postpartum period (22). Similar to other bundles that have been developed and promoted by the Partnership, the hypertension safety bundle is organized into four-domains: Readiness, Recognition and Prevention, Response and Learning. Although the bundle components may be adapted to meet the resources available in individual facilities, standardization within an institution is strongly encouraged.
Severe Hypertension during Pregnancy and Postpartum Period Patient Safety Bundle (23):
Readiness (Every Unit)
- Standards for early warning signs, diagnostic criteria, monitoring and treatment of severe preeclampsia or eclampsia, including order sets and algorithms.
- Unit education on protocols, unit-based drills (with post-drill debriefs).
- Process for timely triage and evaluation of women with hypertension during pregnancy and the postpartum period, including emergency department and outpatient areas.
- Rapid access to medications used for severe hypertension or eclampsia: medications should be stocked and immediately available on labor and delivery and in other areas where patients may be treated; include brief guide for administration and dosage.
- System plan for escalation, obtaining appropriate consultation, and maternal transport, as needed.
Recognition and Prevention (Every Patient)
- Standard protocol for measurement and assessment of blood pressure and urine protein for all women of blood pressure and urine protein for all women during pregnancy and the postpartum period.
- Standard response to maternal early warning signs including listening to and investigating patient symptoms and assessment of laboratory values (e.g., complete blood count with platelets, aspartate transaminase, and alanine transaminase).
- Facility-wide (all areas where pregnant or postpartum women are cared for, labor and delivery, postpartum critical care, and emergency departments etc.) standards for educating women on signs and symptoms of hypertension and preeclampsia prenatally and postpartum.
Response (Every Case of Severe Hypertension or Preeclampsia)
- Facility-wide standard protocols with checklists and escalation policies for management and treatment of:
- Severe hypertension;
- Eclampsia, seizure prophylaxis, and magnesium over-dosage;
- Postpartum presentation of severe hypertension or preeclampsia.
- Minimum requirements for protocol:
- Notification of physician or primary care provider if systolic blood pressure is 160 mm Hg or greater or diastolic blood pressure is 110 mm Hg or greater for two measurements within 15 minutes;
- After the second elevated reading, treatment should be initiated as soon as possible, preferably within 60 minutes of verification;
- Includes onset and duration of magnesium sulfate therapy;
- Includes escalation measures for those unresponsive to standard treatment;
- Describes manner and verification of follow-up within 7 to 14 days postpartum or earlier if with symptoms;
- Describe postpartum patient education for women with preeclampsia.
- Support plan for patients, families, and staff for intensive care until admissions and serious complications of severe hypertension.
Reporting and Systems Learning (Every Unit)
- Establish a culture of huddles for high-risk patients and post-event debriefs to identify successes and opportunities.
- Multidisciplinary review of all severe hypertension and eclampsia patients admitted to an intensive care unit for systems issues.
- Monitor outcomes and process metrics.
Parenteral magnesium sulfate remains the best medication for primary prevention or to reduce the recurrence of eclampsia. Intravenous labetalol and hydralazine are currently recommended as primary antihypertensive agents for acute reductions of critical maternal blood pressure related to preeclampsia (24). Oral nifedipine is acceptable as a first-line antihypertensive medication, particularly when intravenous access is not yet established.
Medications Commonly Used for Hypertension during Pregnancy and Postpartum
Magnesium Sulfate
- Magnesium sulfate not recommended as an antihypertensive agent;
- Should be used for: seizure prophylaxis and controlling seizures in eclampsia;
- Intravenous (IV) bolus of 4 to 6 g in 100 mL over 20 minutes followed by IV infusion of 2 g/hour; continue for 24 hours postpartum;
- Contraindications or relative contraindications: renal failure, myasthenia gravis.
Labetalol
- 20 mg IV bolus followed by 40 mg if not effective within 10 minutes; then, if not effective, 80 mg every 10 minutes; maximum total dose of 300 mg in the first hour;
- Contraindications or relative contraindications: asthma, congestive heart failure.
Hydralazine
- 5 to 10 mg IV every 20 minutes; maximum total dose of 20 mg in the first hour;
- Contraindications or relative contraindications: tachycardia.
Nifedipine
- 10 to 20 mg orally every 30 minutes; maximum total dose of 50 mg in the first hour;
- Note: Nifedipine is not given sublingually;
- Contraindications or relative contraindications: tachycardia.
Facility-wide standards for educating women on signs and symptoms of hypertension and preeclampsia prenatally and postpartum: patient factors such as failure to understand the severity of the illness or delays in reporting symptoms that could represent severe illness have been shown to contribute to preventable maternal deaths from preeclampsia during pregnancy and the first weeks postpartum. Preeclampsia symptoms are frequently nonspecific and thus may not be recognized by the woman and her family as special concerns in pregnancy or early puerperium. Lack of knowledge of specific symptoms can contribute to a delay in seeking care.
Healthcare providers should inform pregnant women about signs and symptoms of preeclampsia, and if these are evident, stress the importance of contacting healthcare providers. These conversations should occur in the context of childbirth education classes, prenatal care visits, during hospitalization, and at postpartum encounters. Strategies should be used to ensure comprehension among women with varying degrees of health literacy. Recommended strategies include using non-medical language wherever possible, reinforcing key issues with print (and video, where available) materials, and requesting information through "teach back" to ensure that the woman and her family members demonstrate understanding.
GLOBAL EFFORTS: Patient Safety and Quality
The global community can increase research activities to better understand the extent to which a harm is preventable and which local- and sector-wide actions will reduce the harm. Research on which methods are most suitable for measuring harm and which mechanisms enable such measurements should also be increased. The WHO has adopted global resolutions, including World Health Assembly Resolution WHA 55.18, to guide efforts to improve safety and quality of care (25). These resolutions alone will not reframe the old narratives into the new one. Practical solutions to guide countries on how to achieve the ideal standards for safety and quality are essential to shift the global dialogue on preventing avoidable causes of human suffering. One measurable step towards new narratives would involve developing standard measures for the major causes of patient harm, such as pressure ulcers, medication errors and diagnostic errors. These standards could be similar to the healthcare-associated-infections action plan made by the United States Center for Disease Control and Prevention (26). Better measurement would enable estimates closer to the true size and scope of the problem and help resolve controversies about current claims about patient safety.
Second, the global health community could encourage coordination of sector-wide efforts to design safe work system. Areas of focus could be better designed medical technologies and tools to reduce the cognitive load that can distract clinicians and lead to error, use of human factors led interventions, and integration and inter-operability of technological systems. Such efforts will require convening different disciplines to better understand how safer systems can be designed. A systems engineering approach, including transdisciplinary experts, starts with a goal, examines the purpose of the healthcare system relative to the goal and then works backward to design a system to achieve that purpose. The approach aligns people, processes, technology and organizational climate to achieve the goal and needs leadership to align stakeholders around a common vision, coordinate efforts, provide resources and incentives and monitor progress. This is the approach other reliability organizations, such as naval aircraft carriers, oil and gas companies, and nuclear power plants, improved. It is therefore encouraging that the WHO Framework on integrated people-centered health services is aligned with this systems approach, specifically by creating an enabling environment to strive for safety and quality improvement (27).
Tackling medication-related harm: The WHO has announced its third global patient safety challenge, which aims to reduce the global burden of iatrogenic medication-related harm by 50% within five years (28). The intention is to match the global research and impact of the two earlier global patient safety challenge: Clean care is safer care and Safe surgery saves lives. The third challenge, Medication without harm, invites health ministers to initiate national plans addressing four domains of medication safety: engaging patients and the public; medication as products; education, training and monitoring of health-care professionals; and systems and practices of medication management. This challenge also commits WHO to using its convening and coordinating powers to drive forward a range of global actions on medication safety (29).
These three priority areas of medication safety that most affect patients, just as hand-hygiene and the surgical checklist are chosen as the flagships of the first two challenges. These three areas are high-risk situations, polypharmacy and transitions of care. Each area is associated with a substantial burden of harm and therefore, if appropriately managed, could reduce the risk of harm to many patients. Certain classes of medications, summarized as high-risk medications in the acronym A PINCH (anti-infective agents; potassium and other electrolytes; insulin; narcotics and other sedatives; chemotherapeutic and immunosuppressive agents; and heparin and anticoagulants), are particularly liable to produce adverse reactions. They tend to have a narrow therapeutic index, meaning that small dosing errors can cause catastrophic outcomes. Focusing on certain key classes of medications has enabled investigators to develop interventions that reduce inadvertent harm caused by these medications. Such interventions can involve low-technology solutions, such as patient medication diaries, or harness the potential of digital technology, as with clinical decision support systems linked with electronic health records (30).
As people tend to live longer, receive treatment for more than one condition at a time and have access to an increasing number of therapeutic options, they tend to take multiple medications. This intake increases the likelihood of drug interactions. Elderly patients may also find it difficult to adhere to complex regimens, increasing the likelihood of patient-induced errors. Progress has been made in identifying medication history and drug-drug combinations that are particularly problematic, enabling risk-stratification and risk-reduction approaches through, for example, de-prescribing initiatives in Canada and the USA. However, these initiatives are only addressing a part of problem of polypharmacy (31). Reducing medication-related harm in the field of transitions of care is the third priority area. Failure to effectively communicate information on medicines and/or underlying risk factors may cause medication errors when patients move between care settings (e.g. from primary to hospital care) and/or between care providers within the same setting (e.g. from out-patient respiratory to out-patient cardiovascular clinics). Initiatives designed to improve communications across such boundaries include standard operating procedures to support medication reconciliation such as WHO's High 5s Project, pharmacist review of patients following admission and discharge from hospitals, summary of care records detailing principal diagnoses, allergies and medication(s), and shared cloud-based applications and electronic health records (32).
The three early priorities of the third global patient safety challenge are not mutually exclusive; many patients may be exposed to risks from a combination of adverse reactions, polypharmacy and miscommunication. Healthcare professionals should focus particularly on those patients who are at higher risk of death or serious illness because of medication-related harm. Making progress across these areas will require politicians and healthcare leaders to prioritize medication safety - as was achieved in the first two challenges. The context in which medication-related occurs across a range of care settings needs to be clearly understood. Implementing measures to reduce this harm will need to include educating and empowering patients and care-takers; developing tools to assist frontline healthcare professionals; and engineering new systems of care to create resilience against the factors that predispose to the risk of medication errors (33).
STRATEGIES FOR IMPROVING DIALOG
Organizational silence undermines a team's ability to develop patient safety protocols and procedures, learn as a team, and maintain quality and safety to improve patient care. Despite important progress in interdisciplinary collaboration in obstetrics, this study suggests that there is room for improvement regarding organizational silence across all the professions involved in labor and delivery, including physicians, midwives, and nurses (34). These findings are consistent with studies in labor-and-delivery units and other settings indicating that hierarchy, disruptive behavior, and lack of perceived support from management for expressing concerns undermine patient safety and that these problems cut across professional boundaries (34). To make a difference in patient care, quality, and morale, labor-and-delivery professionals need to acquire the skills to voice their concerns directly to the involved clinicians in a timely and respectful fashion and be supported by their healthcare organizations when they do so. Clear accountability and commitment from all parties at this critical intersection of individual and organizational responsibility will lead to a safer and more satisfying environment for both patients and healthcare professionals.
- Implement a formal safety program that includes assessment of safety culture, addresses teamwork training, and provides a structure for setting, tracking and achieving measurable improvement goals. It is a well-established practice to measure change-management success with baseline evaluation of outcomes and regular post-treatment assessment. However, outcomes do not capture buy-in and optimism, invaluable in creating lasting improvement, and teamwork training alone is typically not successful without clinician and administrative buy-in.
- Establish the infrastructure for cultural change with a program that provides local control of improvement targets within a broader context of safety learning and evaluation. This evaluation should include opportunities for regular feedback and learning through near-miss and adverse event review.
- Set clear behavioral standards. Specify both the prompt to act and the form of the action that should be taken. When people are told what to look for and how to respond when they see it, they are far more likely to follow-through.
- Build personal motivation. The personal desire to speak up and resolve these difficult situations must be powerful enough to overcome any reluctance or fear.
- Build personal ability. People need to improve their skills for speaking up in these challenging situations. Currently they fear that speaking up will undermine their working relationships and create conflicts in front of patients. They need to know how to bring their concerns in ways that are respectful, minimize defensiveness, and do not provoke conflict.
- Build social motivation and ability. The right people need to lead this change or the old norms will reassert themselves.
- Build structural motivation. Make sure people do not feel punished when they speak up in frank, honest, and respectful ways.
- Build structural ability. Create opportunities for people to speak up and discuss their concerns. These discussions have to occur but need a safe time and safe space. They cannot interrupt or derail the labor and delivery process itself.
- Combine multiple sources of influence. Organizational silence does not have a single root cause, so no single solution will be effective. Strategies that combine multiple strategies to build motivation and ability at the personal, social, and structural levels are far more successful.
Summary
Patient safety is the cornerstone of high-quality health care. Much of the work defining patient safety and practices that prevent harm have focused on negative outcomes of care, such as mortality and morbidity. Health care providers are critical to the surveillance and coordination that reduce such adverse outcomes. Much work remains to be done in evaluating the impact of healthcare provider's care on positive quality indicators, such as appropriate self-care and other measures to improved health status. Although much progress has been made, there is still much work to be done to reduce iatrogenic harm. Key to future improvement is engaged clinical and organizational leadership that must drive a shift in culture and help transform individual experts into expert teams. Several important levers have identified, including fundamental reform in medical education, which can help accelerate this change. The optimal strategy for improving dialog is not known and would likely vary from unit to unit. Our suggestions above contain areas for improving dialog within labor-and-delivery teams. These suggestions draw on research from a wide variety of disciplines. Our data show that communication regarding safety concerns in labor and delivery settings is clearly an area in need of further study.
Implementation of the bundle elements as described above can be facilitated through several targeted free and open-access resources, which the Women's Health and Education Center (WHEC) is developing with its partners. This alliance has short, animated staff training e-learning modules for each of these bundle elements. This national and international program also provides multiple resources and both live and web-based implementation support. One of the goals of these bundles, such as this one, is to improve the readiness of facilities to care for women who present with severe hypertension, to enable them to better recognize women with these conditions, to improve their ability to respond in a timely and appropriate manner, and to facilitate learning from their experience through accurate reporting. Implementation of bundles such as this has the potential to reduce maternal morbidity and mortality from this often devastating condition that threatens safe motherhood.
The obstetrician and gynecologist practices in an environment where emergencies will occur. Preparation for these situations requires allocation of resources and supplies, planning, and collaboration. Inpatient emergencies can be mitigated by a rapid response team that has designated roles, streamlined communication, prompt access to emergency supplies, and ongoing education and training. The criteria used to activate a rapid response team must be defined and disseminated among potential activators. A protocol with standardized interventions and onsite drills will improve the care given in an emergency. The exact nature of the protocol will vary widely depending on the work environment and resources available. Prompt recognition of and response to critical clinical scenarios, teamwork, and training enhance patient safety and mitigate the severity of adverse outcomes.
Suggested Reading
- World Health Organization (WHO)
WHO Surgical Safety Checklist
http://www.who.int/patientsafety/topics/safe-surgery/checklist/en/ - Women's Health and Education Center (WHEC)
Medical Liability: Current Status and Patient Safety
http://www.womenshealthsection.com/content/heal/heal018.php3 - Centers for Disease Control and Prevention (CDC)
Patient Safety: What You Can Do to be a Safe Patient
https://www.cdc.gov/HAI/patientSafety/patient-safety.html - UN University (UNU)
UNU-WIDER Working Paper; 2017
Changing the narratives for patient safety
https://www.wider.unu.edu/sites/default/files/Publications/Working-paper/PDF/wp2017-142.pdf
References
- The Joint Commission Sentinel event statistics data - root causes by event type (2004-2012). Sentinel Event Statistics, 2013. Available at: https://www.jointcommission.org/facts_about_patient_safety/ Accessed 26 July 2017
- Making health care safer: a critical analysis of patient safety practice, evidence report/methodology assessment. No. 43, July 2001. AHRQ Publication No. 01-E057. Rockville MD: Agency for Healthcare Research and Quality. Available at: www.ahrq.gov/clinic/ptsafety/summary.htm Accessed 1 August 2017
- Aspden P, Corrigan J, Wolcott J, et al. Editors. Patient safety: achieving a new standard of care. Washington, DC: National Academies Press; 2004
- National Quality Forum. Standardizing a patient safety taxonomy: a consensus report. Washington, DC: National Quality Forum; 2006
- World Alliance for Patient Safety, launched October 27, 2004, Washington DC. Available at: www.who.int/patientsafety/about/en/index.html Accessed 10 August 2017
- Gluck PA. Medical error theory. Obstet Gynecol Clin North Am. 2008;35:11-17, vii
- Gluck PA. Patient safety: some progress and many challenges. Obstet Gynecol 2012;120:1149-1159
- AHRQ, Quality indicators users' guide: patient safety indicators (PSI) composite measure. Rockville, MD; 2012. Available at: www.qualityindicators.ahrq.gov Accessed 15 August 2017
- Fin R, Yule S. Leadership for safety: industrial experience. Qual Saf Health Care 2004;13(suppl. 2):ii45-51
- The Joint Commission. Sentinel event alert, Issue 57: leadership committed to safety. March 1, 2017. Available at: https://www.jointcommission.org/assets/1/18/SEA_57_Safety_Culture_Leadership_0317.pdf Accessed on 2 August 2017
- Leonard M. and Frankel A. How can leaders influence a safety culture? The Health Foundation Thought Paper. May 2012
- Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 2012;120:1029-1036
- American College of Obstetricians and Gynecologists. Committee Opinion. Preparing for clinical emergencies in obstetrics and gynecology. Obstet Gynecol 2014;123:722-725
- Singh S. Mc Glennnan A, England A, et al. A validation study of the CEMACH recommended modified early obstetric warning system (MEOWS). Anesthesia 2012;67:12-18
- Mahlmeister LR. Best practices in prenatal care: the role of rapid response teams in perinatal units. J Perinat Neonatal Nurs 2006;20:287-289
- Jones DA, De Vita MA, Belloma R. Rapid response teams. N Engl J Med 2011;365:139-146
- Agency for Healthcare Research and Quality. TeamSTEPPS®: national implementation. Available at: http://teamstepps.ahrq.gov/abouttoolsmaterials.htm Accessed on 1 September 2017
- Al Kadri HM. Obstetric medical emergency teams are a step forward in maternal safety! Emerg Trauma Shock 2010;3:337-341
- Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systematic review. Lancet 2006;367:1066-1074
- Royal College of Obstetricians and Gynecologists. Reducing the risk of thrombosis and embolism during pregnancy and the puerperium. Green-top Guideline No. 37a. Available at: http://www.rcog.org.uk/globalassets/documents/guidelines/gtg-37a.pdf Accessed on 15 August 2017
- Robison E, Heyborne K, Allshouse AA, et al. Implementation of a risk-based heparin protocol for postpartum venous thromboembolism prevention. Obstet Gynecol 2017;130:262-269
- The National Partnership for Maternal Safety. Hypertension in pregnancy maternal safety bundle. Available at: https://www.safehealthcareforeverywoman.org Accessed on 23 August 2017
- Bernstein PS, Martin JN, Barton JR, et al. National Partnership for Maternal Safety: consensus bundle on severe hypertension during pregnancy and the postpartum period. Obstet Gynecol 2017;130:347-357
- Emergent therapy for acute-onset, severe hypertension during pregnancy and the postpartum period. Committee Opinion No. 692. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;129:e90-95
- Resolution WHA 55.18. Quality of care: Patient Safety. In: Fifty-fifty World Health Assembly, Geneva, 18 May 2002. Geneva: World Health Organization; 2002. Available at: http://apps.who.int/gb/archive/pdf_files/WHA55/ewha5518.pdf?ua=1 Accessed on 7 August 2017
- Department of Health and Human Services. Action plan to prevent healthcare-associated infections. Atlanta: Centers for Disease Control and Prevention; 2009. Available at: https://stacks.cdc.gov/view/cdc/5872 Accessed on 7 August 2017
- WHO Framework on integrated people-centered health services. Geneva: World Health Organization; 2016. Available at: http://www.who.int/patientsafety/en/ Accessed on 7 August 2017
- Patient safety. WHO global patient safety challenge: medication without harm. World Health Organization; 2017. Available at: http://www.who.int/patientsafety/medication-safety/en Accessed on 9 August 2017
- Donaldson LJ, Kelley ET, Dhingra-Kumar N, et al. Medication without harm: WHO's third global patient safety challenge. Lancet 2017;389:1680-1681
- Thomas SK, McDowell SE, Hodson J, et al. Developing consensus on hospital prescribing indicators of potential harms amenable to decision support. Br J Clin Pharmacol 2013;76(5):797-809
- Tannenbaum C, Martin P, Tambly R, et al. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: The EMPOWER cluster randomized trial. JAMA 2014;174(6):890-898
- Patient Safety. High 5's: standard operating procedures. Geneva: World Health Organization; 2017. Available at: http://www.who.int/patientsafety/topics/high-5s/en Accessed on 23 August 2017
- Sheikh A. Dhingra-Kumar N, Kelley E, et al. The third global patient safety challenge: tackling medication-related harm. Bull World Health Organ 2017;95:546-546A
- Maxfield DG, Lyndon A, Kennedy HP, et al. Confronting safety gaps across labor and delivery teams. AJOG 2013;208:402-408
Publicado: 12 October 2017
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


