Urodynamic Assessment: Patient Evaluation & Equipment
WHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC).
The term urodynamics means observation of the changing function of the lower urinary tract over time. The purpose of an urodynamic assessment is to reproduce the patient's symptoms or usual voiding pattern. By making the appropriate measurements and observations, the underlying physiology becomes apparent. The lower urinary tract has but two functions, the storage and timely expulsion of urine. The bladder fills (at low pressure) with urine from the kidneys and when the urge to void is felt, micturition is postponed until a socially convenient time. During micturition, the sphincter relaxes, the bladder contracts, and the bladder empties. When evaluating a patient with serious clinical disturbance of the lower urinary tract, it is important to understand that one single test cannot reveal everything about the entirety of function of this area. This makes it necessary to use the combined results of a variety of urodynamic assessment procedures in order to understand the effect of various pathological entities on the bladder and the urethra. Urodynamic studies of the lower urinary tract evaluate the dynamic functional activities of the bladder, the sphincter and the interrelation of these two organs during the voiding act itself. This dynamic functional integration of activities determines the normalcy or abnormalcy of the lower urinary tract. Urodynamic or radiologic studies alone or in combination provide useful information in the study of detrusor function. It provides valuable data on bladder function for the healthcare providers to make the best recommendations for treatment.
The purpose of this document is to gain an overall perspective of the urodynamic assessment and have a basic understanding of the principles involved and what to be done looking for with different patient populations. It gives an overview of the procedures to assist healthcare providers in conducting urodynamic assessment. Obtaining a good medical history, concentrating on urologic complaints, is critical to do before embarking on urodynamic assessment. Urodynamics encompasses all the diagnostic modalities used in the evaluation of bladder and urethral function. It describes a number of complimentary tests of varying degrees of complexity that can be performed individually or in combination depending on the clinical circumstances. It has improved our ability to select therapy that addresses the underlying pathophysiology in a rational way. Advances in urodynamics and video-urodynamics has improved our understanding of the normal and abnormal functions of the bladder and sphincter.
Pre-urodynamic Evaluation:
The initial urodynamic assessment should include a comprehensive history and physical examination. Routine laboratory tests that include urinalysis and culture and serum creatinine should be obtained. An elevated serum creatinine may herald significant upper urinary tract deterioration in an otherwise asymptomatic patient. A specific diagnosis of voiding dysfunction based on symptoms alone is unreliable for a myriad of reasons. Considerable overlap may exist between urgency and stress incontinence symptoms, and also between urgency and obstructive symptoms. Patients with neurologic conditions may have serious underlying abnormalities with few symptoms.
History: The general history should include questions relevant to neurologic and congenital abnormalities and information on previous urinary functions and relevant surgery. Information must be obtained on medication with known or possible effects on the lower urinary tract. The general history should also include assessment of menstrual, sexual and bowel function, and obstetric history. After the urologic history, thorough medical, surgical, gynecologic, neurologic, and obstetric histories should be obtained. Certain medical and neurologic conditions, such as diabetes, stroke, and lumbar disk disease, may cause urinary incontinence. Furthermore, strong coughing associated with chronic pulmonary disease can markedly worsen symptoms of stress incontinence. A history of hysterectomy, vaginal repair, pelvic radiotherapy, or retropubic surgery should alert the physician to the possibility of prior surgical trauma to the lower urinary tract.
Urinary Diary: Patient histories regarding frequency and severity of urinary symptoms are often inaccurate and misleading. Urinary diaries are more reliable and require the patient to record volume and frequency of fluid intake and voiding, usually a 1- to 7-day period. Episodes of urinary incontinence and associated events or symptoms such as coughing or urgency are noted. The number of times voided each night and any episodes of bedwetting are recorded the next morning. The maximum voided volume also provides a relatively accurate estimate of bladder capacity. The physician should review the frequency / volume charts with the patient and corroborate or modify the initial diagnostic impression.
Physical Examination:
Besides a general physical, urologic and gynecologic examination, the examination should include the assessment of perineal sensation, the perineal reflexes supplied by the sacral segments S2-S4, and anal sphincter tone and control. Vulvar and vaginal atrophy consistent with hypoestrogenemia suggests that the urethra and peri-urethral tissues are also atrophic. The presence and severity of anterior vaginal relaxation, including cystocele and proximal urethral detachment and mobility, or anterior vaginal scarring, are estimated. Associated pelvic support abnormalities, such as rectocele, enterocele, and uterovaginal prolapse, are noted. The rectal examination, further evaluates for pelvic pathology and fecal impaction, the latter of which may be associated with voiding difficulties and incontinence in elderly women.
Neurologic Examination: Urinary incontinence may be the presenting symptom of neurologic disease. The screening neurologic examination should evaluate mental status as well as sensory and motor function of both lower extremities. Disorders associated with mental status aberrations that may produce neurologic abnormalities include senile and pre-senile dementia, brain tumors, and normal pressure hydrocephalus. Spinal cord lesions produce varied and characteristic patterns of sensory loss depending on the portion of the spinal cord affected. Complete spinal cord transaction or transverse myelitis is associated with complete sensory loss below the level of the lesion including sense of pain, light touch, and vibration. Coordinated bladder function is usually disrupted with complete spinal cord injury with resultant detrusor hyperreflexia and external-sphincter dyssynergia. In posterior column syndrome such as tabes dorsalis, only vibratory sensation in the lower extremities is lost. This may result in sensory neurogenic bladder wherein the patients progress toward urinary retention simply because they lack the sensation of bladder filling or fullness. The bladder gradually stretches, and the detrusor decompensates. Motor functions -- specific muscles important in the neurologic examination include the tibialis anterior (L4-S1), gastrocnemius (L5-S2), and extensors of the toes (L4-S2). These muscles may be tested through dorsiflexion (extension) of the foot, plantar flexion of the foot, and extension of the toes, respectively. Paralysis of the tibialis anterior is typically manifested by a foot drop. Alterations in muscle tone are important signs of neurologic disease. Hypotonicity may result from peripheral nerve lesions, loss of proprioception (tabes dorsalis), or various myopathies. Hypotonia of the extremities is also present typically in spinal shock or following a cerebrovascular accident (cerebral shock). Hypertonicity usually indicates a supra-segmental lesion, most commonly one involving the pyramidal or extra-pyramidal tracts.
Reflexes: The cremasteric reflex (L1-L2) is elicited by stroking the inner thigh and results in ipsilateral elevation of the testicle. The anal reflex (S 2-S5) is elicited by lightly stroking the perianal skin and results in anal contraction. The bulbocavernosus reflex in men is elicited by squeezing the glans penis (not the body of penis) and monitoring external anal sphincter contraction. In women, the glans clitoris is used. The spinal cord segments subserving these reflexes are primarily S2-S4. These reflexes have been demonstrated in more than 70% of healthy individuals. Absence of this reflex is suggestive of a segmental or peripheral nerve lesion and provides corroboration of a neurogenic basis for urodynamic abnormalities such as detrusor areflexia. Reflex activity of the perineal activity striated muscles may also be elicited from the vesicourethral mucosa by tugging on an indwelling urethral catheter. Light stimulation of the perianal skin will also produce external anal sphincter contraction (anal wink). Sacral reflexes are specialized cutaneous reflexes that are of particular relevance to urodynamics because they permit direct assessment of the sacral spinal cord segments. The external anal sphincter may be considered to be representative of all the perineal striated muscles. The tone of this muscle is assessed by the rectal examination. Presence of voluntary contraction indicates integrity of the pelvic floor innervation. Preservation of tone in the absence of voluntary contraction indicates a suprasacral lesion, whereas diminished tone implies a sacral or peripheral nerve abnormality.
Perineal Pad Tests:
Perineal pad weighing may be used when one wants to document objectively the presence and amount of urine loss. The test should approximate activities in daily life and should evaluate as long as a period as possible, yet be practical. A 1-hour period of testing is recommended and can be extended for additional 1-hour periods if the result of the first test is not considered representative of the symptoms by either the patient or the physician. Alternatively, the test can be performed after filling the bladder to a defined volume or at home over a 24-hour period. The total amount of urine lost during the test period is determined by weighing a collecting device such as absorbent pad. A typical test schedule is started without the patient voiding and with drinking approximately 500 mL of fluid. A period of walking, coughing, exercise, and hand-washing is done. At the end of the 1-hour test the collecting device is removed and weighed. Two critical variables determines the sensitivity of pad weighing -- the amount of fluid in the bladder during exercise and the type of activity used to generate increased intraabdominal pressure. Pad weighing has acceptable test-retest reliability and is easy to perform in a clinical setting. However, it has low sensitivity and poor correlation between pad gain and videographic assessment of incontinence severity. These shortcomings have limited acceptance of pad weighing as a routine part of the evaluation of incontinence. Phenazopyridine hydrochloride (Pyridium) is sometimes used to aid clinicians in differentiating urinary continence from incontinence in women with disturbing vaginal wetness. Red-orange staining is taken as evidence that urine loss has occurred.
Q-Tip Test:
Placement of a cotton swab in the urethra to the level of the vesical neck and measurement of the axis change with straining can be used to demonstrate urethral mobility. To perform the Q-tip test, a sterile, lubricated cotton-tipped applicator is inserted transurethrally into the bladder, then withdrawn slowly until definite resistance is felt, indicating that the cotton tip is at the bladder neck. This is best accomplished with the patient in the supine lithotomy position during a pelvic examination. The resting angle of the applicator stick in relation to the horizontal is measured with a goniometer or protractor. The patient is then asked to cough and perform a Valsalva maneuver, and the maximum straining angle from the horizontal is measured. Results are not affected by the amount of urine in the bladder. Care should be taken to ensure that the cotton tip is not in the bladder or at the mid-urethra because this results in a falsely low measurement of urethral mobility. Although maximum straining angle measurements greater than 30 degrees are generally considered to be abnormal, few data are available to differentiate normal from abnormal measurements. Urethral mobility in continent women is probably related to age, parity, and support defects of the anterior vaginal wall.
Radiologic Assessment and Ultrasonography:
Patients with neurologic disease and others at risk for upper tract deterioration should undergo baseline renal radiographic investigations. An adequate evaluation of the upper urinary tracts includes either an intravenous pyelogram (IVP) or a renal ultrasound. Lateral cystourethrography in the resting and straining view can identify mobility or fixation of the bladder neck, funneling of the bladder neck and proximal urethra, and degree of cystocele. The voiding component can identify a urethral diverticulum, fistula, obstruction, or vesicoureteral reflux. Video-cystourethrography allows a dynamic assessment of the anatomy and function of the bladder base and urethra during retrograde filling with contrast material and during voiding. It is most helpful in sorting out causes of complex incontinence problems. However, it is invasive, expensive, and not widely available. For these reasons, other methods are usually used to measure urethral mobility in incontinent women.
Ultrasonography is an alternative method of evaluating the urethrovesical anatomy. When compared to bead-chain cystourethrography, fluoroscopy, and the Q-tip test, perineal and vaginal ultrasonography accurately displays descent of the urethrovesical junction, opening of the bladder neck, and detrusor contractions. This technique appears to hold promise as a non-invasive and accurate method of evaluating the position and mobility of the urethrovesical junction and proximal urethra in incontinent women.
Laboratory Tests:
Few laboratory tests are necessary for the evaluation of incontinence. A clean midstream or catheterized urine sample should be obtained for dipstick urinalysis. Urine culture and sensitivity should be obtained when the dipstick test indicates infection. Acute cystitis can present with multiple irritative symptoms, such as dysuria, frequency, urgency, incontinence, and voiding difficulty. In these cases, treatment of the infection usually eradicates the symptoms. However, bacteriuria is often asymptomatic in the elderly. If seems reasonable to examine the urine for infection in all incontinent patients and if bacteriuria is found, to prescribe appropriate antibiotics and reevaluate the patient in several weeks. Blood testing (BUN, creatinine, glucose, and calcium) is recommended if compromised renal function is suspected or if polyuria (in the absence of diuretics) is present. Urine cytology is not recommended in the routine evaluation of the incontinent patient. However, patients with hematuria (2 to 5 RBC/hpf) or acute onset of irritative voiding symptoms in the absence of urinary tract infection require cystoscopy and cytology to exclude bladder symptoms.
Indications for Urodynamic Tests:
The physician must recognize that even under the most typical clinical situations, the diagnosis of incontinence based only on clinical evaluation may be uncertain. This diagnostic uncertainty may be acceptable if medical or behavioral treatment (as opposed to surgery) is planned because of the low morbidity and cost of these treatments and because the ramifications of non-cure (continued incontinence) are not severe. When surgical treatment of stress incontinence is planned, urodynamic testing is recommended to confirm the diagnosis. As noted, consultation should be considered for complex cases that may require urodynamic testing or surgical treatment. Whenever objective clinical findings do not correlate with or reproduce the patient's symptoms, urodynamic testing is indicated for diagnosis. Finally, when trials of therapy are used, patients must be followed up periodically to evaluate response. If the patient fails to improve to her satisfaction, appropriate further testing is indicated.
Equipment:
Commercially available cystometers can be broadly classified into single-channel and multi-channel machines (subtracted cystometry). Single-channel cystometry involves the placement into the bladder of a pressure-measuring catheter that produces an electronic signal, creating a graph on a recording device. Multi-channel cystometry relies on the measurement of both abdominal (Pabd) and intravesical pressures (Pves), thereby enabling one to distinguish changes in intraabdominal pressure from changes in intravesical pressure. Abdominal pressure can be measured via either transrectal or transvaginal catheters. We prefer vaginally placed catheters because they are more comfortable and easier to clean and maintain, and measurements are not cluttered by rectal peristalsis. Electronic subtraction of intraabdominal from intravesical pressure allows for the calculation of true detrusor pressure (Pdet). Subtracted cystometry may be enhanced further by additional measurement of urethral pressure (Pure). This measurement allows for the calculation of urethral closure pressure (Pucp), which is the difference between urethral and bladder pressures. Certain machines also allow for the simultaneous measurement of electromyographic (EMG) activity and the performance of flow studies. Choosing urodynamic equipment is not very different from choosing other equipment for the clinician's office, but there are certain differences. Urodynamics is an interactive examination that permits the clinician not only to look, but also to evaluate physiology. The testing sequence and the specific tests to perform depend on a variety of factors including the patient's symptoms, mobility, previous treatments and surgeries and, the interest, expertise, and equipment available to the clinician. Multi-channel video-urodynamics offers the most accurate snapshot of normal and abnormal physiology and has the least chance of causing unrecognized artifacts or misdiagnoses. It is also the most expensive, time consuming, and requires more personnel. It does not, however, require more expertise. In fact, just the opposite is true. A single-channel cystometrogram requires more subtleties of clinical experience and knowledge precisely because only one pressure is being recorded. In a multi-channel system, an increase in vesical pressure can be instantly recognized as either a detrusor contraction or an increase in abdominal pressure simply by glancing at the respective channels. It is not so easy with a single-channel cystometers. The basic tool of the urodynamicist is the cystometrogram (CMG); no urodynamic evaluation is complete without a CMG. Next in importance are the uroflow and an estimation of postvoid residual urine. Thus, a cystometer and flowmeter are essential features of any urodynamic studies. For those interested in the engineering aspects and parameters of urodynamic testing, they should look at the International Continence Society Working Party on Urodynamic Equipment.
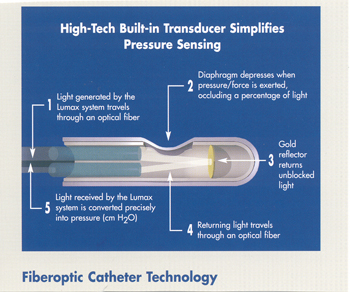
Urodynamic catheters and catheter size: For cystometry, catheter size and type does not affect the outcome of the study. A Foley catheter or a specialized urodynamic catheter provides the same kind of clinical information. One practical point, the larger the catheter, the faster and easier it is to infuse fluid. The only limitation is the comfort (or discomfort) caused by the catheter itself. In practice, catheters up to 12 or 14 Fr are well tolerated. Whenever uroflow is measured with a urethral catheter in place, as in detrusor pressure / uroflow studies, the design and size of the catheter is clinically relevant. Two kinds of urodynamic catheters for pressure flow studies exist: 1) a double or triple lumen catheter for bladder filling and measurement of vesical and/or urethral pressure, and 2) a two catheter system, one for filling and one to measure vesical pressure. The larger the catheter, the greater the likelihood that it will influence the results of the study by: 1) causing discomfort, 2) artifactually increasing detrusor pressure, and 3) artificially decreasing uroflow. A 10 Fr catheter can cause an elevation in detrusor voiding pressure and a decrease in maximum flow rate compared with a 4 Fr catheter in men with prostatic obstruction. No difference in voiding pressure and flow rate exists between the 10 Fr and 4 Fr urodynamic catheters in non-obstructed urethra. Fiberoptic catheters utilize a proven and patented fiberoptic technology that simplifies the procedure and allows for the easy integration of urodynamics into any practice. At the speed of light, bladder and abdominal pressures are measured through fiberoptic catheter for an accurate result. They are available in 2 sizes: 10 Fr or 7 Fr.

Reporting and Equipment Calibration:
Urodynamic information can be displayed two ways: as an image on a video monitor or as lines on a strip-chart. Some units can store the information in either analog or digital form (or both), and can select appropriate segments for the final hard copy. The main advantage to digital storage is that the information can be entered directly into a data base; this is more useful in research. A desirable feature for the clinician is the ability to compress the hard copy of the analog tracing so that it may be displayed on a standard-sized form. This does away with the problem of dealing with long, unwieldy tracing form the strip-chart recorder. Some units have built-in computers that can do word processing as well as data storage and retrieval. This is particularly useful for writing standardized reports and may be combined with other functions such as referral letters, and billing. A common and serious problem in urodynamics is failure to maintain the equipment properly. Laboratories with excellent equipment can obtain incorrect result because the equipment is calibrated improperly. Malfunction of equipment certainly can and does occur. Catheter leaks, air bubbles in a closed system, improper electrical grounding, mechanical failure, and inaccurate instrument calibration are all potential sources of error. Equipment must be maintained in a clean state, sterilized properly, and used correctly. Universal precautions should be practiced in all patient encounters.
Summary:
Urodynamic studies, in concert with an accurate history and physical examination, are the most useful clinical tools available for the evaluation of lower urinary tract dysfunction. However, the accuracy of measurements and their physiologic relevance can limit the clinical applications of the information obtained. The clinicians performing urodynamics should have a special interest and expertise in the physiology and neurophysiology of the lower urinary tract. A significant problem in urodynamic evaluation is an inappropriate interpretation of an observation. Often, it is not the measurement that is in error, but rather the interpretation. The clinician must recognize both the value and the limitation of each segment of an urodynamic study. A reliable measure is one that has a small error component and does not fluctuate randomly from one moment to the next. The most important aspect of an urodynamic study is that it be accurate and clinically relevant. The urodynamicist is reminded the urodynamic evaluation is an interactive process intended to reproduce the patient's symptoms, and, that by appropriate measurements and observations, a correct diagnosis can be obtained in majority of patients. The interpretation of the urodynamic study should never be independent of the overall clinical picture. If the results don't make sense, they are probably wrong.
Suggested Reading:
- Miller EA. Preoperative urodynamic evaluation may predict voiding dysfunction in women undergoing pubovaginal sling. J Urol 2003;169:2234-2237
- Urinary Incontinence Treatment Network (UITN) Continence Treatment Centers [http://www.niddk.nih.gov/patient/uitn/uitn.htm] (accessed 3 January 2008)
- Pollak JT, Jenkins P, Kopka S et al. Effect of genital prolapse on assessment of bladder neck mobility by the Q-tip test. Obstet Gynecol 2003;101:662-665
- Karram MM, Walters MD. Urogynecology and reconstructive pelvic surgery. Third Editions. St. Louis: Mosby, 2007.
- Blaivas J, Chancellor M. Atlas of urodynamics. Baltimore: William & Wilkins, 2007.
- Benson JT. Clinical neurophysiological techniques in urinary and fecal incontinence. In: Ostergard DR, Bent AE. Ostergard's Urogynecology and pelvic floor dysfunction. Philadelphia: Lippincott Williams & Wilkins, 2003.
- Bhatia NN. Dynamics of voiding in women. Curr Opin Obstet Gynecol 2000;12:383-386
- Takacs EB, Zimmern PE. Recommendations for urodynamic assessment in the evaluation of women with stress urinary incontinence. Clin Prac Urol 2006;10:544-550
- Arya LA, Myers DL, Jackson ND. Office screening test for intrinsic urethral sphincter deficiency: pediatric Foley catheter test. Obstet Gynecol 2001;97:885-889
- Jackson SL, Scholes D, Boyko EJ et al. Predictors of urinary incontinence in a prospective cohort of postmenopausal women. Obstet Gynecol 2006;108:855-862
Published: 9 February 2009
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


