Detección e intervención de la pérdida auditiva del recién nacidoWHEC Boletín Práctica Clínica y Gestión de los proveedores de salud. Educación subvención prevista de Salud de la Mujer y el Centro de Educación (WHEC). Hearing loss can affect a child’s ability to develop communication, language, and social skills. The earlier children with hearing loss start getting services, the more likely they are to reach their full potential. If you are a parent and you suspect your child has hearing loss, trust your instincts and speak with your child’s doctor. Most children hear and listen to sounds at birth. They learn to talk by imitating the sounds they hear around them and the voices of their parents and caregivers. But that is not true for all children. In fact, about 2 or 3 out of every 1,000 children in the United States (US) are born with detectable hearing loss in one or both ears. More lose hearing later during childhood. Children who have hearing loss may not learn speech and language as well as children who can hear. For this reason, it is important to detect deafness or hearing loss as early as possible. Because of the need for prompt identification for childhood hearing loss, universal newborn hearing screening programs currently operate in all U.S. states and most U.S. territories. With help from the federal government, every state has established an Early Hearing Detection and Intervention Program. As a result, more than 96% of babies heave their hearing screened within 1 month of birth. The purpose of this document is to review the importance of baby’s hearing screening, how it is done and the types of intervention services available. The most important time for a child to learn language is in the first 3 years of life, when the brain is developing and maturing. In fact, children begin learning speech and language in the first 6 months of life. Research suggests that children with hearing loss who get help early develop better language skills than those who do not. IntroductionA hearing loss can happen when any part of the ear is not working in the usual way. This includes the outer ear, middle ear, inner ear, hearing (acoustic) nerve, and auditory system. The acoustic nerve sends sound information from ear to the brain and the auditory system processes sound information as it travels from the ear to the brain. According to the Centers for Disease Control and Prevention (CDC), currently around 98% of newborns are screened for hearing loss in the US, annually. Since more than 50,000 infants who are deaf and hard-of-hearing have been identified within the first year of life and have had the opportunity to receive early intervention services that can help them reach their full potential. Before 1993, fewer than 1 in 10 newborns in the US, were screened for hearing loss, but now nearly all are screened. According to CDC in 2017 (1):
DefinitionsThe functions, skills and abilities of voice, speech, and language are related. Some dictionaries and textbooks use the terms almost interchangeably. But for scientists and medical professionals, it is important to distinguish among them. Voice (or Vocalization): It is the sound produced by humans and other vertebrates using the lungs and the vocal folds in the larynx, or voice box. Voice is not always produced as speech, however. Infants babble and coo; animals bark, moo, whinny, growl, and meow; and adult humans laugh, sing and cry. Voice is generated by airflow from the lungs as the vocal folds are brought close together. When air is pushed past the vocal folds with sufficient pressure, the vocal folds vibrate. If the vocal folds in the larynx did not vibrate normally, speech could only be produced as a whisper. Your voice is as unique as your fingerprint. It helps define your personality, mood, and health. According to the National Institute on Deafness and Other Communication Disorder (NIDCD), approximately, 17.9 million adults in the US have trouble using their voices. Disorders of the voice involve problems with pitch, loudness, and quality. Pitch is the highness or lowness of a sound based on the frequency of the sound waves. Loudness is the perceived volume (or amplitude) of the sound, while quality refers to the character or distinctive attributes of a sound. Speech: Humans express thoughts, feelings, and ideas orally to one another through a series of complex movements that alter and mold the basic tone created by voice into specific, decodable sounds. Speech is produced by precisely coordinated muscle actions in the head, neck, chest, and abdomen. Speech development is a gradual process that requires years of practice. During this process, a child learns how to regulate these muscles to produce understandable speech. In the US, roughly 5% of children have noticeable speech disorders, according to NIDCD. The majority of these speech disorders have no known cause. One category of speech disorder is fluency disorder, or stuttering, which is characterized by a disruption in the flow of speech. It includes repetitions of speech sounds, hesitations before and during speaking, and the prolonged emphasis of speech sounds. More than 15 million individuals in the world stutter, most of whom began stuttering at an early age. The majority of speech sound disorders in the preschool years occur in children who are developing normally in all other areas. Speech disorders also may occur in children who have developmental disabilities. Language: It is the expression of human communication through which knowledge, belief, and behavior can be experienced, explained, and shared. This sharing is based on systematic, conventionally used signs, sounds, gestures, or marks that convey understood meanings within a group or community. Recent research identifies "windows of opportunities" for acquiring language - written, spoken, or signed - that exist within the few years of life. According to NIDCD, between 6 and 8 million individuals in the US have some form of language impairment. Disorders of language affect children and adults differently. For children who do not use language normally from birth, or who acquire an impairment during childhood, language may not be fully developed or acquired. Language disorders also are found in adults who have failed to develop normal language skills because of mental retardation, autism, hearing impairment, or other congenital or acquired disorders of brain development. Many adults acquire language disorders because of stroke, head injury, dementia, or brain tumors. Signs and Symptoms of Hearing LossThe signs and symptoms of hearing loss are different for each child. Even if a child passed a hearing screening before, it is important to look out for the following signs. Signs in babies: Does not startle at loud noises; Does not turn to the source of a sound after 6 months of age; Does not say single words, such as “dada” or “mama” by 1 year of age; Turns head when he or she sees you but not if you only call out his or her name. This sometimes is mistaken for not paying attention or just ignoring but could be the result of partial or complete hearing loss; Seems to hear some sounds but not others. Signs in children: Speech is delayed; Speech is not clear; Dose not follow directions. This sometimes is mistaken for not paying attention or just ignoring but could be the result of a partial or complete hearing loss; Often stays “Huh?” and Turns the television volume up too high. Babies and children should reach milestones in how they play, learn, communicate, and act (2). A delay in any of these milestones could be a sign of hearing loss or other developmental problem. CDC’s Development Milestones – from 2 months to 5 years; available @ Screening and Diagnosis of Hearing LossHearing screening is a test to tell if people might have hearing loss. Hearing screening is easy and not painful. In fact, babies are often asleep while being screened. It takes a noticeably short time – usually only a few minutes. Babies:
Older Babies and Children
Screening TestsTwo different tests are used to screen for hearing loss in babies. Your babies can rest and sleep during both tests. 1. Otoacoustic Emissions (OAE): It tests whether some parts of the ear respond to sound. During this test, a soft earphone is inserted into your baby’s ear canal. It plays sounds and measures an echo response that occurs in ears with normal hearing. If there is no echo, your baby might have hearing loss.  2. The auditory brain stem response (ABR) or Brainstem Auditory Evoked Response (BAER) Test: It tests how the auditory nerve and brain stem (which carry sound from the ear to the brain) respond to sound. During this test, your baby wears a small earphones and has electrodes painlessly placed on his or her head. The electrodes adhere and come off like stickers and should not cause discomfort. Because this test does not rely on a person’s response behavior, the person being tested can be sound asleep during the test. ABR focuses only on the function of the inner ear, the acoustic (hearing) nerve, and part of the brain pathways that are associated with hearing. For this test, electrodes are places on the person’s head (similar to electrodes placed around the heart when and electrocardiogram (EKG) is done), and brain wave activity in response to sound is recorded. Full Hearing TestAll children who do not pass a hearing screening should have a full hearing test. This test is also called an audiology evaluation . an audiologist, who is expert trained to test hearing, will do the full hearing test. In addition, the audiologist will also ask questions about birth history, ear infection and hearing loss in the family. Some of the test the audiologist might use include: Otoacoustic Emissions (OAE); ABR or BAER test (stated above); and behavioral audiometry evaluation. 3. Behavioral Audiometry Evaluation: It will test how a person responds to sound overall. Infants and toddlers are observed for changes in their behavior such as sucking a pacifier, quieting, or searching for the sound. They are rewarded for the correct response by getting to watch an animated toy (this is called visual reinforcement audiometry). Sometimes older children are given a more play-like activity (this is called conditioned play audiometry). Behavioral Audiometry Evaluation tests the function of all parts of the ear. The person being tested must be awake and must response to sounds heard cooperative during this tests. AnatomyA hearing loss happen when any part of the ear or auditory (hearing) system is not working in the usual way – Outer Ear, Middle Ear, Inner Ear, Auditory (ear) Nerve, Auditory (hearing) System. 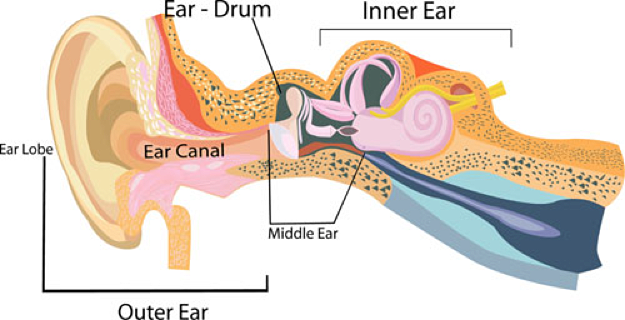 Outer ear: It is made up of - the part we see on the sides of our heads, known as pinna, the ear canal, and the eardrum, sometimes called the tympanic membrane, which separates the outer and middle ear. Middle ear: It is made up of - the eardrum and three small bones called ossicles that send the movement of the eardrum to the inner ear. Inner ear: It is made up of - the snail shaped organ for hearing known as the cochlea, the semicircular canals that help with balance, and the nerves that go to the brain. Auditory (ear) nerve: This nerve sends sound information from the ear to the brain. Auditory (hearing) System: The auditory pathway processes sound information as it travels from the ear to the brain so that our brain pathways are part of our hearing. Journey of Sound to the Brain Types of Hearing LossThere are four types of hearing loss:
Degree of Hearing LossIt can range from mild to profound.
Descriptions of Hearing LossHearing loss can also be described as:
Is Your Child "At Risk" for Hearing Loss?If you checked one or more boxes below, your child may be at risk for hearing loss.
Causes and Risk FactorsHearing loss can happen anytime during life – from birth to adulthood. Following are some of the things that can increase the chance that a child will having hearing loss (1,2). 1 out of 4 cases of hearing loss in babies is due to maternal infections during pregnancy, complications after birth, and head trauma. For example, the child:
For about 1 out of 4 babies born with hearing loss, the cause is unknown. Genetic Cause The cochlea (the part of the ear that changes sounds in the air into nerve signals to the brain) is a complex and specialized part of the body that needs many instructions to guide its development and function. These instructions come from genes. Changes in any one of these genes can result in hearing loss. The GJB2 gene is one the genes that contains the instructions for a protein called connexin 26; this protein plays an important role in the functioning of the cochlea. In some populations about 40% of newborns with a genetic hearing loss who do not have a syndrome, have a mutation of the GJB2 gene. Details: https://www.cdc.gov/ncbddd/hearingloss/freematerials/parentsguide508.pdf Cytomegalovirus & Hearing Loss In this study delayed-onset and progression of sensorineural hearing loss (SNHL) in children with congenital CMV continued to occur throughout adolescence (3). However, the risk of developing SNHL after age 5 years among case-patients was not different than in uninfected children. Overall, 2% of case-patients developed SNHL that was severe enough for them to be candidates for cochlear implantation. In this study (3), from age 3 months to 5 years, the prevalence of SNHL doubled among case-patients from 7% to 14% but remained at 0% among controls. The burden of CMV-related SNHL is substantial considering the potential impact of SNHL on children's development and academic achievement and their need for ongoing audiologic monitoring and interventions. There is estimate that 5% of children with asymptomatic congenital CMV infection, about 900 children annually, have SNHL >70 dB HL in at least 1 ear by age 12 months, and half of these children meet current candidacy criteria for cochlear implantation (4). As cochlear implant technologies and indications for their use continue to evolve, the number of children with asymptomatic congenital CMV infection and SNHL who might be considered candidates for cochlear implants could increase. Newborn screening for congenital CMV infection has potential to identify children at risk for CMV-related SNHL who currently go unrecognized and who might benefit from earlier intervention (5). Additional investigation into age of onset and risk factors for SNHL in children with asymptomatic congenital CMV infection are needed to inform the evaluation of the potential costs and benefits of CMV screening. Auditory Neuropathy When their hearing sensitivity is tested, people with auditory neuropathy may have normal hearing or hearing loss ranging from mild to severe. They always have poor speech-perception abilities, meaning that they have trouble understanding speech clearly. People with auditory neuropathy have greater impairment in speech perception than hearing health experts would predict based upon their degree of hearing loss on a hearing test. For example, a person with auditory neuropathy may be able to hear sounds but would still have difficulty recognizing spoken words. Sounds may fade in and out or seem out of sync for these individuals. Risk factors of auditory neuropathy: There are several ways that children may acquire auditory neuropathy. Some children diagnosed with auditory neuropathy experienced particular health problems before or during birth or as newborns.
Meningitis and Hearing Loss Congenital Unilateral Hearing Loss (UHL) In an attempt to diagnose and intervene earlier in children with hearing loss, the Joint Committee on Infant Hearing (JCIH) endorsed a "1-3-6 Plan," in which all infants will be screened no later than 1 month, have confirmation of hearing loss by 3 months, and receive intervention by 6 months (13). Despite these initiatives, nearly half of all infants who do not pass the initial hospital hearing screen do not receive timely, appropriate follow up care. A study found that the presence of co-occurring birth defects prolonged the time to initial hearing screening, resulting delays to diagnosis and intervention (14). Risk factors for UHL (15):
The importance of congenital birth defects in this population is two-folds. First, the presence of a comorbid birth defect increases the chances that a child may need prolonged mechanical ventilator support. Multiple studies have demonstrated that mechanical ventilation greatly increases the likelihood of SNHL (16). The study also reported that application of mechanical ventilation can significantly damage the peripheral segment of the hearing tract. Second, the presence of a comorbid birth defect has been shown to lead to an increase in time to hearing screening, diagnosis, and intervention (17). In this study, a 3-year cohort study, 39,000 infants in the neonatal intensive care unit were 16.4 times more likely to miss the initial hearing screening and nearly 6 times more likely to miss their rescreen compared with infants in a well-baby nursery (18). It is important to recognize children at risk for hearing loss and to perform screening and confirmatory testing in a timely manner despite the possible multitude of distracting congenital birth defects (19). The absence of risk factors does not preclude the development of UHL. Further studies are needed to define the etiology underlying UHL and better define the risk factor associations. Early Hearing Screening Program for Infants and Children in U.S.Prior to the establishment of a federal universal newborn infant hearing screening program in 1999, less than 10% of newborns in the U.S. were screened for hearing loss. As a result, 47% of children born with hearing loss were not diagnosed until their third birthday or later, missing a crucial period for language acquisition. In fact, children begin learning speech and language in the first six months of life, which is why early identification of hearing loss is critical (20). Research suggests that children with hearing loss who get help early develop better language skills than those who do not.  In 2017 the Early Hearing Detection and Intervention (EHDI) law re-authorizes Health Resources and Service Administration (HRSA) to continue funding awards to states, territories, and healthcare providers to support continuous improvement of EHDI programs. These projects help to identify effective strategies to address screening, loss to follow-up diagnosis and services, enrollment into early intervention services, and family engagement. Project grants are also awarded to organizations to improve family-to-family support systems and to educate healthcare professionals who provide services to children who are deaf or hard-of-hearing (21). On October 18, 2017, President Trump signed into law S. 652, EHDI Act (PL 115-71). The law amends the Public Health Service Act to re-authorize until 2022 a federal program administration by the U.S. Department of Health and Human Services (HHS). Three HHS agencies - the HRSA, the CDC, and the National Institutes of Health (NIH) - will continue a long-standing partnership to coordinate and advance a national program for the early identification and diagnosis of hearing loss and intervention services for deaf and hard-of-hearing newborns and infants. In addition, the law authorizes specific changes to the federal program, such as expanding the program to include young children who are at risk of losing their hearing during childhood from infection, harmful noise exposure, or genetic causes. The law also encourages EHDI research programs at NIH through projects supported by the National Institute on Deafness and Other Communication Disorders (NIDCD). The NIDCD is committed to supporting biomedical research to improve both early hearing detection and intervention and hearing loss management, including screening, treatment, and rehabilitation (22). The law will allow for continued support of research on hearing aids, cochlear implants, speech perception and production, and language (both spoken and signed). Collectively, HRSA, CDC, and NIH will enhance coordination so the federal EHDI program in U.S. and its territories, continues to ensure that infants who are deaf or hard-of-hearing are identified as early as possible and receive effective and timely interventions (23). These collaborations are critical to improving outcomes for affected children. HHS agencies will continue to promote essential services in order to minimize the negative impact that undiagnosed hearing loss can have on children’s speech, language, academic, social, and emotional development. AphasiaAphasia is a disorder that results from damage to portions of the brain that are responsible for language. For most people, these areas are on the left side of the brain. It usually occurs suddenly, often following a stroke or head injury, but it may also develop slowly, as the result of a brain tumor or a progressive neurological disease. The disorder impairs the expression and understanding of language as well as reading and writing. Aphasia may co-occur with speech disorders, such as dysarthria or apraxia of speech, which also result from brain damage. 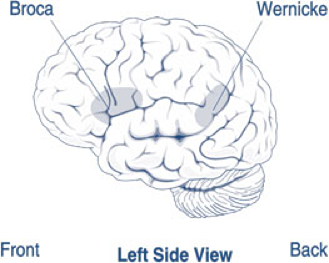 About 1 million people in U.S. currently have aphasia, and nearly 180,000 Americans acquire it each year (24). There are two broad categories of aphasia: fluent and non-fluent, and there are several types within these groups. Damage to the temporal lobe of the brain may result in Wernicke's aphasia (shown in the picture above), the most common type of fluent aphasia. People with Wernicke's aphasia my speak in line, complete sentences that have no meaning, adding unnecessary words and even creating made-up words. Another hallmark of this type of aphasia is difficulty understanding speech. The most common type of non-fluent aphasia is Broca's aphasia (see picture above). People with Broca’s aphasia have damage that primarily affects the frontal lobe of the brain. They often have right-sided weakness or paralysis of the arm and leg because the frontal lobe is also important for motor movements. People with Broca's aphasia my understand speech and know what they want to say, but they frequently speak in short phrases that are produced with great effort. They often omit small words, such as "is," "and" and "the." Global aphasia, results from damage to extensive portions of the language areas of the brain. Individuals with global aphasia have severe communication difficulties and may be extremely limited in their ability to speak or comprehend language. They may be unable to say even a few words or may repeat the same words or phases over and over again. They may have trouble understanding even simple words and sentences. There are other types of aphasia, each of which results from damage to different language areas in the brain. Conduction aphasia - these people have difficulty repeating words and sentences even though they understand them and can speak fluently. Anomic aphasia - people have difficulty naming objects even though they know what the object is and what it may be used for. Sometimes, blood flow to the brain is temporarily interrupted and quickly restored. When this type of injury occurs, which is called a transient ischemic attack, language abilities may return in a few hours or days. Diagnosis: Most individuals will undergo a magnetic resonance imaging (MRI) or computed tomography (CT) scan to confirm the presence of a brain injury and to identify its precise location. If the physician suspects aphasia, the patient is usually referred to a speech-language pathologist, who performs a comprehensive examination of the person's communication abilities. The person's ability to speak, express ideas, converse socially, understand language, and read and write are all assessed in detail. Aphasia therapy aims to improve a person's ability to communicate by helping him or her to use remaining language abilities, restore language abilities as much as possible, and learn other ways of communicating, such as gestures, pictures, and use of electronic devices. Individual therapy focuses on the specific needs of the person, while group therapy offers the opportunity to use new communication skills in a small-group setting. Noise Induced Hearing Loss (NIHL)NIHL can be caused by a one-time exposure to an intense "impulse" sound, such as an explosion, or by continuous exposure to loud sounds over an extended period of time, such as noise generated in a woodworking shop. Recreational activities that can put you at risk for NIHL include target shooting and hunting, snowmobile riding, listening to MP3 players at high volume through earbuds or headphones, playing in a band, and attending loud concerts. Sound is measured in units called decibels. Sounds at or below 70 A-weighted decibels (dBA), even after long exposure, are unlikely to cause hearing loss. However, long, or repeated exposure to sounds at or above 85 dBA can cause hearing loss. The louder the sound, the shorter the amount of time it takes for NIHL to happen. Researchers have estimated that as many as 17% of teens (ages 12 to 19) have features of their hearing test suggestive of NIHL in one or both ears (25). Based on a 2011 - 2012 CDC study involving hearing tests and interviews with participants, at least 10 million adults (6%) in the U.S. under age 70 - and perhaps as many as 40 million adults (24%) - have features of their hearing test that suggest hearing loss in one or both ears from exposure to loud noise. 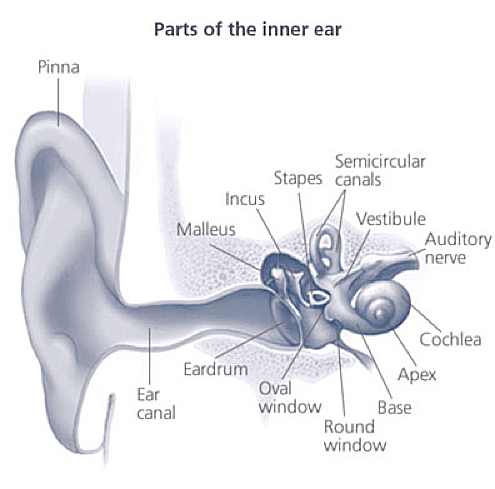 Once the vibrations cause the fluid inside the cochlea to ripple, a traveling wave forms along the basilar membrane. Hair cells - sensory cells sitting on top of basilar membrane ride the wave. As the hair cells move up and down, microscopic hair-like projections (known as stereocilia) that perch up on top of the hair cells bump against on overlying structure and bend. Bending causes pore-like channels, which are at the tips of the stereocilia, to open up. When that happens, chemicals rush into the cell, creating an electrical signal. The auditory nerve carries this electrical signal to the brain, which translates it into a sound that we recognize and understand. NIHL is the only type of hearing loss that is completely preventable. If you understand the hazards of noise and how to practice good hearing health, you can protect your hearing for life. Protect the ears of children who are too young to protect their own. Known which noises can cause damage (those at or above 85 dBA. Noisy Planet is a national public education campaign designed to increase awareness among parents of children ages 8 to 12 about the causes and prevention of noise-induced hearing loss (26). 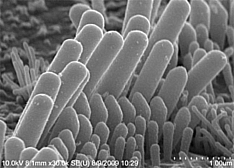 Most NIHL is caused by the damage and eventual death these hair cells. Unlike bird and amphibian hair cells, human hair cells do not grow back. They are gone for good. Loud noise exposure can also cause tinnitus - a ringing, buzzing, or roaring in the ears or head. Tinnitus may subside over time but can sometimes continue constantly or occasionally throughout a person’s life. Hearing loss and tinnitus can occur in one or both ears. PreventionFollowing are tips for parents to help prevent hearing loss in their children:
Types of InterventionsThere are different types of communication options and interventions available for children with hearing loss. With help from healthcare providers and intervention specialists, families are able to select the options that best meet their needs. These are some of the possible options:
Early Intervention and Special Education Early Intervention (0-3 years) Special Education (3 - 22 years) Early Hearing Detection and Intervention (EHDI) Program TechnologyTechnology does not "cure" hearing loss but may help a child with hearing loss to make the most of their residual hearing. Hearing Aids: It makes sounds louder. They can be worn by people of any age, including infants. Babies with hearing loss may understand sounds better using hearing aids. This may give them the chance to learn speech skills at a young age. There are many styles of hearing aids. They can help many types of hearing losses. A young child is usually fitted with behind-the-ear style hearing aids because they are better suited to growing ears. See the figure 7 below. Bone-Anchored Hearing Aids: This type of hearing aid can be considered when a child has either a conductive, mixed, or unilateral hearing loss and is specifically suitable for children who cannot otherwise wear 'in the ear' hearing aids.  |