Fetal Alcohol Syndrome: Recognition & PreventionMaternal alcohol abuse is associated with impaired fetal growth; virtually all neonates with fetal alcohol syndrome (FAS) will exhibit significant growth restriction. It is unknown whether a threshold-effect exists for alcohol, but effects on the fetus are related to the amount consumed. Women are more likely to be hidden drinkers and frequently under report alcohol use, especially during pregnancy. Tests to detect the problem in women must include questions about tolerance, which are not included in the most commonly employed screen. Pregnant women are more likely to be screened than non-pregnant women. Although the vulnerability of the fetus is an important concern, the lives of non-pregnant women also have compelling value, and there is much evidence to suggest that women who abuse alcohol or use illicit drugs have co-existing or pre-existing conditions (ie, mental health disorders, domestic violence, stress, childhood sexual abuse, poverty, and lack of resources) that put them in a vulnerable status. Additionally, failure to diagnose and treat alcohol and substance abuse with the same evidence-based approach applied to other chronic illnesses reduces patient's access to health services and resources. The purpose of this document is to understand the recognition and prevention of fetal alcohol syndrome (FAS). The physicians should counsel patients presenting with drug or alcohol problems and refer them to an appropriate treatment resource when available. Physicians who detect the serious medical condition of addiction (drugs and/or alcohol) are obligated to intervene during pregnancy or pre-conceptional counseling. On the one hand, no person has a right to use illegal drugs, and a pregnant woman has a moral obligation to avoid use of both illicit drugs and alcohol in order to safeguard the welfare of her fetus. On the other hand, effective intervention with respect to substance and alcohol abuse by a pregnant or a non-pregnant woman requires that a climate of respect and trust exist within the physician-patient relationship. Patients who begin to disclose behaviors that are stigmatized by society may be harmed if they feel that their trust is met with disrespect. Terminology:Fetal alcohol spectrum disorders (FASD) is caused by the effects of maternal alcohol consumption during pregnancy. Fetal alcohol syndrome (FAS) is the most clinically recognizable form of FASD and is characterized by a pattern of facial anomalies, prenatal and postnatal growth retardation, and functional or structural central nervous system (CNS) abnormalities. The consequences are life-long, and the behavioral and learning difficulties are often greater than the degree of neuro-cognitive impairment. Alcohol related neurodevelopment disorder also is a clinically recognizable diagnosis in the continuum of FASD and describes the clinical outcome when the facial features typical of FAS are absent (1). FASD is more strongly associated with higher levels of alcohol consumption. Epidemiology:Prenatal alcohol exposure is regarded as a leading preventable cause of birth defects and developmental disabilities in the United States. Alcohol abuse among women of child-bearing age is prevalent in the United States, with approximately 1 in 5 non-pregnant women reporting binge drinking (5 or more drinks on any one occasion) and 1 in 25 pregnant women reporting binge drinking (2). Early identification of children with fetal alcohol syndrome (FAS) has shown to enhance their long-term outcomes, neurodevelopment and physical growth. Therefore, identifying women who are at high-risk for an alcohol exposed pregnancy and intervening with them before conception is an essential strategy for preventing alcohol exposed pregnancies and birth defects and developmental disabilities. FASD may affect up to 1% of the US population and 10% women between 18 to 44 years of age use alcohol during pregnancy and 2% engage in "binge drinking". Many institutions do not have appropriate protocols in place for intervention and referral. Fetal alcohol syndrome (FAS) following maternal ethanol ingestion has recently been described, with an incidence varying from 1 in 1,500 to 1 in 600 live births, depending apparently on variations in drinking practices. Alcohol crosses placenta easily. Instances of newborns showing alcoholic withdrawal symptoms have been reported, but only in infants born to chronic alcoholics who drank heavily during pregnancy. Moreover, the chronic alcoholic may suffer from malnutrition, to the extent that the craving for alcohol exceeds the desire for food. Diagnostic Features of Fetal Alcohol Syndrome (FAS) and Fetal Alcohol Spectrum Disorders (FASD):It is one of the most frequent recognizable causes of mental retardation in the United States, a tragedy that could be avoided. FASD and FAS are non-hereditary; alcohol causes neuronal damage and cell loss in the fetal brain through direct action as a toxin. No prenatal period has been shown to be safe from the deleterious effects of alcohol exposure in any trimester, even before the time of a pregnancy test. Women should be advised not to drink from the time of conception to birth. Prenatal exposure also increases the risk of pregnancy complications such as intraventricular hemorrhage and white matter brain damage in preterm neonates. Virtually all neonates with FAS and FASD have significant growth restriction (3). Brief out-line of diagnostic criteria is based on facial dysmorphia; growth problems and central nervous system abnormalities. Facial Dysmorphia: small palpebral fissures, a thin upper lip (thin vermillion border), a long smooth philtrum are most commonly seen facial anomalies. Other findings may include a flat mid-face, ptosis (dropping) of the eyelids, epicanthal folds, an upturned nose with a flat nasal bridge, under-developed ears. Clinodactyly (curved fifth finger) and camptodactyly (the upper palmar "hockey stick" crease), hirsutism and cardiac defects, and microcephaly are commonly present. Growth Problems: prenatal or postnatal height or weight, or both, at or below the 10th percentile, documented at any one point in time (adjusted for age, sex, gestational age, and race or ethnicity). Central Nervous System Abnormalities: head circumference (OFC) at or below 10th percentile adjusted for age and sex and clinically significant brain abnormalities is observable through imaging in newborns and children with FAS and FASD. Cognitive deficits and behavioral anomalies such as attention-deficit/ hyperactivity disorder typically become more apparent in school-aged children with FASD and usually persist into adolescence and adulthood, whereas facial findings among the subset with FAS may become less characteristic. Newborns and Children with Fetal Alcohol Syndrome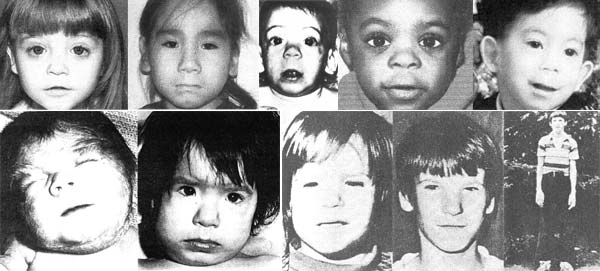 Newborns and Children with Fetal Alcohol Syndrome Screening for women at risk for an alcohol-exposed pregnancy:Screening instruments have been developed and validated for use in pregnant women and non-pregnant women. Many questionnaires have been developed like T-ACE and T-WEAK and are useful in identifying the alcohol and substance abuse problems (4). Some preliminary screening questions suggested with Yes and No check-boxes to pregnant and non-pregnant women are:
Intervention, Referral and Management:Pre-conceptional women may benefit from discussions that include pregnancy postponement and effective contraception to avoid an alcohol-exposed pregnancy while she attempts to reach goals of alcohol reduction or abstinence. Follow-up should be conducted for every high-risk woman, and any woman who is unable to achieve her drinking goals should receive stepped-up care, including referral to formal treatment programs or community groups that provide support to women seeking to reduce hazardous alcohol use patterns. FAS and all other conditions are included under the umbrella of fetal alcohol spectrum disorders. These conditions are entirely preventable as long as a pregnancy is an alcohol-free pregnancy (5). Referral to a multidisciplinary team (ie, dysmorphologist/clinical geneticist, developmental pediatrician, mental health professional, social worker, and educational specialist) often is necessary for diagnosis because the growth, CNS, and facial features of FASD can overlap other syndromes and disorders. Even in patients who clearly have met diagnostic criteria, referral allows complete assessment for an individualized management plan. It is important to provide patients with health education materials containing messages that are clear and brief and do not require the user to navigate algorithms and text. Prevention:Approximately 8% of women of childbearing age are at risk of pregnancy, and half of them are actively trying to become pregnant. However, half of all pregnancies are unplanned and many women will not know they are pregnant during the early weeks of gestation and will continue consuming alcohol at levels that result in the birth of a child with fetal alcohol spectrum disorders (FASD). Therefore, identifying who are at risk for an alcohol exposed pregnancy and intervening with them before conception is an essential strategy for preventing alcohol-exposed pregnancies. Social services are needed to ensure a safe home environment and provide parental education. Early identification and intervention results in significantly improved outcomes. Fortunately, early cessation of alcohol use may result in amelioration of some its teratogenic effects. Even low levels of alcohol consumption cannot be recommended during pregnancy (6). Besides individual variation of "threshold dose" there are confounding effects of maternal age, other drug and environmental exposures, and pregnancy complications. A diagnosis of FAS meets the "presumptive diagnosis" requirements of Part C of the Individuals with Disabilities Education Act, allowing children younger than three years to receive services even if their test results fall in the normal range. After three years of age, eligibility for services often depends on demonstration of a specific functional deficit. Breast Feeding:Although alcohol passes freely into breast milk, reaching concentrations approximating maternal serum levels, the effect on the infant is probably insignificant except in rare cases or at very high concentrations. The toxic metabolite of ethanol, acetaldehyde, apparently does not pass into milk even though considerable levels can be measured in mother's blood. Maternal levels have to reach 300 mg/dl before mild sedation might be seen in the baby. Possibility of severe hypoprothrombic bleeding, a pseudo-Cushing syndrome, and an effect on the milk-ejecting reflex have been reported in nursing infants of alcoholic mothers. The American Academy of Pediatrics considers maternal ethanol use compatible with breast-feeding, although adverse effects may occur. Drinking and Reproductive Health:If there is a potential for her to put her pregnancy at risk from alcohol use, a brief intervention, using motivational interviewing techniques, should be used. The approach is to let the patient know that she is drinking more than most women (she probably does not know that) and empower her to make the "right" decision. Because alcohol use presents a risk to pregnancy, she might choose effective contraception or, if she's becoming or is pregnant, she could choose to quit drinking. The goal is harm reduction, by separating alcohol from pre-pregnancy. It is important not to make her feel guilty and to follow-up with her at successive visit. Randomized clinical trials showing that this works have been published, and more studies testing even briefer interventions are underway (7). There is increasing susceptibility as women age for full fetal alcohol syndrome, alcohol-related birth defects, and alcohol-related neurodevelopmental disorders, so a previous apparently normal pregnancy outcome, despite alcohol exposure, is not a guarantee of a good outcome for current pregnancy. The occasional abusive drinker or alcohol-dependent woman should be referred to a substance-abuse specialist. However, for most patients, obstetricians and gynecologists should provide the following advice (8):
Obstetricians and gynecologist can play a major role in identifying and addressing alcohol use during pregnancy. We should be formally screening all reproductive-age patients for risk drinking, doing a brief intervention, or if appropriate, referring the patient. At the absolute minimum, we should be strongly advising our patients not to drink alcohol during pregnancy. Summary:Treat the patient with a substance abuse problem with dignity and respect in order to form a therapeutic alliance. Protect confidentiality and the integrity of the physician-patient relationship whenever possible within the requirements of legal obligations, and communicate honestly and directly with patients about what information can and cannot be protected. Recognize that the most effective safeguard for children is treatment for family members who have a substance abuse problem. Alcohol and substance abuse is a common medical condition that can have devastating physical and emotional consequences for women and their children. The traditional role of healer, the contemporary role of medical expert, and the newer role of primary care physician all require obstetricians -- gynecologists to develop an evidence-based knowledge about methods for detection and treatment of alcohol and substance abuse. The close working relationship between the physician and the patient that is both a goal of care and a means to improved health outcomes, offers tremendous potential to influence patients' lifestyles positively. Common barriers to universal screening questions, brief intervention, and referral to treatment can and should be addressed. Physicians have an ethical obligation to learn and use techniques for universal screening questions, brief intervention, and referral to treatment in order to provide patients and their families with medical care that is state-of-art, comprehensive, and effective. Acknowledgment: This chapter is very likely to appeal to any person concerned with human development. We express our sincere thanks to Department of Obstetrics and Gynecology, St. Elizabeth's Medical Center, Boston, MA (USA) for the assistance with preparation of manuscript. Resources:
References:
|