Circuncisión masculina del recién nacidoWHEC Boletín Práctica Clínica y Gestión de los proveedores de salud. Educación subvención prevista de Salud de la Mujer y el Centro de Educación (WHEC). Male circumcision is surgical removal of skin covering the tip of penis. This procedure is fairly common for male newborns, in certain parts of the world, including in the United States of America (USA). Circumcision after the newborn period is possible, but at that time, it is a more complex procedure. For some families, circumcision is a religious ritual. The procedure can also be a matter of family tradition, personal hygiene or preventive health care. For others, however, circumcision seems unnecessary or disfiguring. In the USA, newborn male circumcision is the fourth most common surgical procedure - behind cataract removal, cesarean delivery, and joint replacement (1). This surgical procedure, which dates to ancient times, is chosen for medical, personal, or religious reasons. It is performed on 77% of males born in the USA and on 42% of those born elsewhere who are living in this country (2). If it is performed in USA, it depends not only on the parent's race, ethnic background, and religion, but also on the region and state. In the USA, circumcision rates range varies from 74% in the Midwest to 30% in the West, and in between are the Northeast (67%) and the South (61%) (3). The purpose of this document is to review common questions and controversy of newborn male circumcision and provide evidence-based answers to them. Circumcision is not without controversy in USA. Some claim that it is unnecessary cosmetic surgery, and that it is genital mutilation, or that the patient cannot choose it or object to it, or that it decreases sexual satisfaction. Parents and families should start thinking about circumcision before the infant is born. The Women's Health and Education Center (WHEC) recommends, to make an informed choice. Parents of all male infants should be given accurate information about the potential risks and benefits of the procedure. Parents should also have an opportunity to discuss the decision with healthcare providers. BackgroundOver the past 20 years, a growing body of evidence has demonstrated real medical benefits of circumcision. In 2012, the American Academy of Pediatrics (AAP), which issued a task force report concluding that the health benefits of circumcision outweigh its risks and justify access to the procedure (3). However, the report stopped short of recommending circumcision on the routine basis. According to its statement "although health benefits are not great enough to recommend routine circumcision for all male newborns, the benefits of circumcision are sufficient to justify access to this procedure for families choosing it and to warrant third-party payment for circumcision of male newborns." It is important to note that clinicians routinely counsel parents of the health benefits and risks of male newborn circumcision in an unbiased and accurate manner. The Pros and ConsFor many years, the medical benefits of circumcision were scientifically ambiguous. With no clear answers, some thought that parents should base their decision for or against circumcision not on any potential medical benefit but rather on their family or religious traditions, or on a social standard, that is, what the majority of families in their community do. Opponents have expressed several concerns about circumcision. First, they say, it is painful and unnecessary, and performing it when life has just begun takes the decision away from the adult-to-be, who may want to be uncircumcised as an adult but will not have any recourse. Second, they say circumcision will diminish the adult's sexual pleasure. However, there is no proof this occurs, and it is unclear how the claim could be adequately verified (4). Health benefits of circumcision: Adverse effects of circumcision: Analgesia for CircumcisionAlthough in decades past, circumcision was often performed without any analgesia, in the United States, analgesia is now standard of care. The AAP Task Force on Circumcision formalized this standard in a 2012 policy statement (3). For newborn circumcision, an analgesia can be given in the form of analgesic cream, penile ring block, or dorsal nerve block. Analgesic EMLA cream (a mixture of local anesthetics such as lidocaine 2.5% / prilocaine 2.5%) is easy to use but it is minimally effective in relieving circumcision pain, although some investigators have reported it is efficacious compared with placebo (8). When used, the analgesic cream is applied 30 to 60 minutes before circumcision. EMLA and other lidocaine creams can cause skin color changes of local skin irritation. There is a rare risk with lidocaine creams of causing methaemoglobinaemia (blue-baby syndrome, where the baby's blood lacks sufficient oxygen). However, two trials of EMLA for circumcision pain relief measured methaemoglobin levels and found them normal. The circumcision procedure itself, especially without pain relief, can cause short term effects such as chocking, gagging, and vomiting. Long term effects of circumcision without pain relief are not well understood. Strict comparability between trials was rare. Trials used a variety of indicators to measure baby's pain. Crying time, facial expression, and sweating palms can indicate infant pain, as can increased heart rate, breathing rate, and blood pressure. Both penile ring block and dorsal nerve block with 1% lidocaine are easy to administer and are very effective (9). They are best used with buffered lidocaine, which partially relieves the burning that occurs with injection. With both methods, the smaller the needle used (preferably 30 gauge), the better. These two block methods have different injection sites. For the ring block, small amount of lidocaine (1.0 to 1.5 mL) are given in a series of injections around the entire circumference of the base of the penis. The dorsal block targets the two dorsal nerves located at 10 o'clock and 2 o'clock at the base of the penis. Epinephrine should NOT be used with local analgesia for penile infiltration. Epinephrine has vasoconstrictive properties and it has the potential for necrosis, hence never used for penile infiltration. Penile nerve block technique: 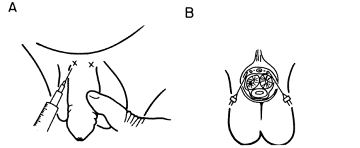 Analgesia can be supplemented with comfort measures, such as a pacifier, sugar water, gentle rubbing on the forehead, and soothing speech (10). Conditions for Safe CircumcisionAs circumcision is not medically required and need not occur in the days immediately after birth, it should be performed only when conditions are optimal:
Circumcision Procedure - An OverviewCircumcision can be performed with the Gomco circumcision clamp, the Mogen circumcision clamp, or the Plastibell circumcision device. Each device works well, provides excellent results, and has its pluses and minuses. Practitioners should use the device with which they are most familiar and comfortable with, and likely it will be the device they used in their training. In the United States, the Gomco clamp is perhaps the most commonly used device. It provides good cosmetic results, and its metal "bell" protects the entire head of the penis. Of the three methods, however it is the most difficult - the partially cut foreskin must be threaded between bell and the clamp frame before the clamp is tightened. In many cases, there is bleeding at the penile frenulum.  The Mogen clamp, another commonly used device, also is used in traditional Jewish circumcisions. Of the three methods, it is quickest, produces the best hemostasis, and is associated with the least discomfort (11). To those unfamiliar with this method, there may seem to be a potential for amputation of the head of the penis, but actually there virtually is no risk, as an indentation on the penile side of the clamp protects the penile head.  The Plastibell device is very easy to use but must stay on until the foreskin becomes necrotic and the bell and foreskin fall off on their own - a process that takes 7 to 10 days. Many patients dislike this method because it is not immediate, and they have to contend with a medical implement during their newborn's first week home.  Electrocautery is not recommended. Some clinicians, especially urologists, use electrocautery as the cutting mechanism for circumcision. A review of literature, however, reveals that electrocautery has not been studied head-to-head against traditional techniques, and that various significant complications - transected penile head, severe burns, meatal stenosis - have been reported (12). It is certainly not a mainstream procedure for neonatal circumcision. Circumcision MethodThe foreskin is a sleeve of tissue which covers the penis. At birth it is tightly attached. By mid-childhood it can be pulled over the penis when the penis is flaccid or retracted back over the shaft of the penis during urination or erection. The common indication for circumcision is cultural or religious desire for circumcision. Other indications (rare):
Circumcision of a newborn boy is usually done before he leaves the hospital. A numbing medication (local anesthesia such as Xylocaine) is injected into the penis to reduce pain. Ring-type clamps are placed around the foreskin, tightened like a tourniquet to reduce bleeding, and the foreskin is removed below the clamp. Sometimes a plastic clamp is used (Plastibell). The Plastibell will fall off in 5 to 8 days, after the surgical site has healed. For both newborns and older children, circumcision is considered a very safe procedure with complete healing expected. Healing time for newborns usually takes about 1 week. Apply petroleum jelly after diaper changes to protect the healing incision. Some initial swelling and yellow crust formation around the incision is normal. Healing time for older children and adolescents may take up to 3 weeks. In most instances, the child will be discharged from the hospital on the day of surgery. 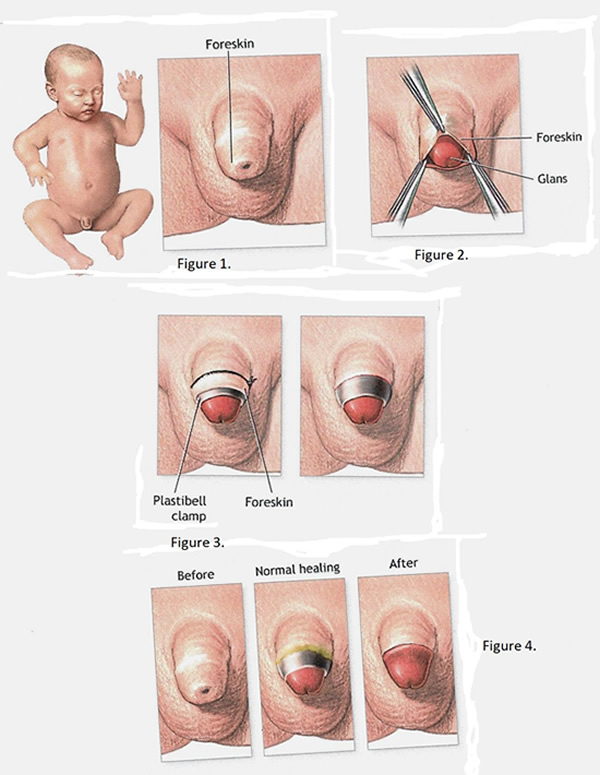 Most clinicians would be reluctant to perform a circumcision in the office or clinic after the baby is 6 to 8 weeks old. If a family desires their son to be circumcised after that time - or a medical condition procedure precludes earlier circumcision - the procedure is best performed by a pediatric urologist in the operating room. For the procedure video in complication situations; please visit the video (13). Complications / Sequelae of CircumcisionThe rate of circumcision complications is very low at 0.2%. That being said, the 3 most common types of complications are - postoperative bleeding, infection, and damage to penis (14).
Other considerations - the procedure contains specialized sensory tissue that is removed during circumcision. Some men believe that the end of the penis becomes less sensitive when the foreskin is removed, and that sexual sensation may be decreased, however, most circumcised males do not describe psychological trauma or decreased sexual function or desire as a result of the procedure (15). Parents should be aware that some health insurance plans do not cover the cost of circumcision. Parents should call their healthinsurance plan directly to find out if the circumcision procedure is covered. What is Jewish Ritual Circumcision?For their newborn's circumcision, Jewish parents may choose a bris ceremony, formally called a brit-milah, in fulfillment of religious tradition. The ceremony involves a brief religious service, circumcision with the traditional Mogen clamp, a special blessing, and an official religious naming rite. The bris traditionally is performed by a mohel, a rabbi or other religious official trained in circumcision. Many parents have the bris done by a mohel who is a medical-doctor. In the United States, the availability of both types of mohels varies. Care of Uncircumcised Penis - information for the parentsIn the first several years of your son's life foreskin will separate from the tip of the penis. Some foreskins separate soon after birth or even before birth, but this is rare. When it happens is different for every child. It may take a few weeks, months, or years. Once this happens, the foreskin can be pulled back away from the tip of the penis. This is called foreskin retraction. Most boys will be able to retract foreskin by the time they are 5 years old, yet others will not be able until the teen years. As a boy becomes more aware of his body he will most likely discover how to retract his own foreskin. But foreskin retraction should never be forced. Until the foreskin fully separates, do not try to pull it back. Forcing the foreskin to retract before it is ready can cause severe pain, bleeding, and tears in the skin. Smegma: when the foreskin separates from the head of the penis, skin cells are shed. These skin cells may look like white, pearl-like lumps under the foreskin. These are called smegma. Smegma is normal and nothing to worry about. Cleaning - a guide for parents: if your son's foreskin separates before he reaches puberty, an occasional retraction with cleansing beneath will do. Once your son starts puberty, he should clean beneath his foreskin as part of his daily routine, just like washing hair and brushing his teeth. Teach your son to clean his foreskin in the following way (16):
WHO Program for Male Circumcision and HIV PreventionThe World Health Organization (WHO) launched the 2018 Manual for Male Circumcision under local anesthesia and other HIV prevention services for adolescent boys and men to support the ongoing delivery of high quality services (17). Since the 2007 WHO and Joint United Nations Programme on HIV/AIDS (UNAIDS) recommendation to add male circumcision as an intervention in a package of services to reduce men's risk of heterosexually acquired HIV, extensive practical experience has been gained and lessons learned. Neonatal and child male circumcision - a global review (18): There is currently increased interest in male circumcision services, since three randomized controlled trials have confirmed that circumcision reduces the risk of acquiring HIV infection in males. Several countries with high prevalence of HIV are now expanding access to safe male circumcision. The immediate focus of circumcision for HIV prevention is on adolescents and adult men, but a longer-term HIV prevention strategy is likely to include the provision of neonatal and child circumcision. This global review (19) shows that circumcision complications are rare when conducted by trained and experienced providers with adequate supplies and in hygienic conditions. However, there is a clear need for comprehensive, ongoing training programs for both medically trained and non-medically trained providers, which should cover all aspects of the procedure and aftercare in order to avoid the current unnecessary morbidity associated with the procedure in many settings. Clinical TrialsA clinical study involves research using human volunteers (also called participants) that is intended to add to medical knowledge. There are two main types of clinical trials (also called interventional studies) and observational studies. ClinicalTrials.gov includes both interventional and observational studies (19). SummaryIn the United States a large percentage of male infants are circumcised. Although circumcision has known medical benefits, the procedure generally is performed for family, religious, or cultural reasons. Existing scientific evidence demonstrates potential medical benefits of newborn male circumcision; however, these data are not sufficient to recommend routine neonatal circumcision. Circumcision is a safe and straightforward procedure but has its risks and potential complications. The exact incidence of complications after circumcision is not known, but data indicate that the rate is low, and the most common complications are local infection and bleeding. Analgesia must be provided if circumcision is performed. Swaddling, sucrose by mouth, and acetaminophen administration may reduce the stress response but are not sufficient for the operative pain and cannot be recommended as the sole method of analgesia. Although local anesthesia and combination preparations of lidocaine and prilocaine provide some anesthesia and combination preparations of lidocaine and prilocaine provide some anesthesia benefit, both ring blocks and dorsal penile blocks have been proved to be more effective. As with most surgeries, the best outcomes are achieved by practitioners who are well trained, who perform the procedure under supervision until their experience is sufficient, and who follow correct protocol during the entire operation. References
|