Prevención de la enfermedad por estreptococos del grupo B en recién nacidos: tratamiento perinatal
WHEC Boletín Práctica Clínica y de gestión para proveedores de atención médica. Educación subvención prevista de Salud de la Mujer y el Centro de Educación (WHEC).
Group B streptococcus (GBS) is the leading cause of newborn infection. It is a common commensal in the gut of humans and in the lower genital tract in women, remains an important cause of neonatal mortality and morbidity. The incidence of early-onset disease has fallen markedly in countries that test women for carriage at 35 – 37 weeks of pregnancy and then offer intrapartum prophylaxis with penicillin during labor. Countries that do not test, but instead employ a risk factor approach, have not seen a similar fall. There are concerns about the effect on the neonatal microbiome of widespread use of antibiotic prophylaxis during labor, but so far the effects seem minor and temporary. Universal screening and antibiotic prophylaxis of all GBS carriers result in increased antibiotic exposure in most of the populations, which might carry its own risks. Therefore, patients should be involved in decisions on whether to be screened or not, is based on identification of risks and benefits. Vaccination against GBS would be acceptable to most women and GBS vaccines are in the early stages of development.
The purpose of this document is to identify limitations of current strategies for antepartum and intrapartum prophylaxis of neonatal early-onset group B streptococcal (GBS) infection. Better strategies are needed to assure timely administration when prophylaxis is indicated. Neonatal sepsis continues to cause a significant proportion of perinatal mortality and long-term morbidity in the term and preterm infant population. The most common single organism that causes early-onset neonatal sepsis is the group B streptococcus (GBS or Streptococcus agalactiae) (1). The present guidelines are designed to lower the risk of GBS early-onset-disease, which is the most common cause of early-onset neonatal sepsis.
What is Group B Streptococcus (GBS)?
Antony van Leeuwenhoek (1632 - 1723) was the first to identify microscopic one-celled organisms, which he called 'animalcules.' He described bacteria of the genus Selenomonas (crescent shaped bacteria from the human mouth) in 1676. The understanding of bacteria was greatly increased by the work of Louis Pasteur (1822 - 1895), but it was Robert Koch (1843 - 1910) who first linked specific microorganisms to particular diseases, such as tuberculosis, cholera and anthrax. A Viennese surgeon Theodor Billroth (1829 - 1894) coined the term Streptococcus to describe a group of bacteria within the order Lactobacillales and phylum Firmicutes. Beta-hemolytic Streptococci are so-called because when they are cultured on blood agar, the red blood cells are lysed and the hemoglobin the cells contained is denatured so that its red color disappears.
Group B beta-hemolytic Streptococci (GBS) are called S. agalactiae (Latin for "without milk") because they cause mastitis in cows. GBS is a facultative gram-positive organism. It is a common bowel commensal in many animals including fish, cattle, and humans, in which it is present in 20 – 40% of adults (2). It can be divided into 10 serotypes based on a serological reaction directed against the polysaccharide capsule, and which are thought to influence virulence and antibiotic resistance. The most frequently identified serotypes that cause invasive disease in neonates are III (60.6%) and Ia (17.3%), whereas type VI (32.7%), Ib (19.4%), and V (19.4%) are the most common cause of invasive disease in adults (3). Serotype VI is the leading type that colonizes pregnant women (35.0%) (3). However, the differences are not currently thought to be sufficient to make them useful in clinical practice.

Figure 1. Group B Streptococcus (GBS) or Streptococcus agalactiae.
Source: CDC
Introduction
The primary risk factor for neonatal GBS early-onset-disease is maternal colonization of the genito-urinary and gastro-intestinal tracts. Vertical transmission usually occurs during labor or after rupture of membranes. Implementation of national guidelines for intrapartum antibiotic prophylaxis has resulted in a reduction in incidence of GBS early-onset-disease of more than 80%, from 1.8 newborns per 1,000 live births in the 1990s to 0.23 newborns per 1,000 live births in 2015 (4).
In 2010, the Centers for Disease Control and Prevention (CDC), in collaboration with several professional groups, including the American College of Obstetricians and Gynecologists (ACOG), issued its third set of GBS prevention guidelines. In 2018, the stewardship of the change for updating the GBS prophylaxis guidelines were transferred from the CDC to ACOG and the American Academy of Pediatrics (AAP). In addition, the American Society of Microbiology maintains standards for laboratory procedures relevant to processing specimens. The key obstetric measures necessary for effective prevention of GBS early-onset-disease continue to include universal prenatal screening by vaginal-rectal culture, correct specimen collection and processing, appropriate implementation of intrapartum antibiotic prophylaxis, and coordination with pediatric care providers.
Background
In 1970s, GBS emerged as an important cause of perinatal morbidity and mortality in newborns (5). Two distinct clinical syndromes of invasive GBS disease in the newborn exist:
- GBS early-onset-disease, which presents within 7 days after birth and occurs secondary to vertical transmission, fetal or neonatal aspiration during labor and birth, or both. It is characterized primarily by sepsis, pneumonia, or less frequently meningitis and is most likely to manifest within the first 12-48 hours after birth (6).
- GBS late-onset disease, presents between 7 days after birth and 2 – 3 months of age. It is characterized by bacteremia, meningitis, or less commonly, organ or soft tissue infection. Late-onset disease is primarily acquired by horizontal transmission from the mother, but also can be acquired from hospital sources or from individuals in the community (7).
Prevalence
Approximately 50% of women who are colonized with GBS will transmit the bacteria to their newborns. In absence of intrapartum antibiotic prophylaxis, 1 – 2% of these newborns will develop GBS early onset disease (8). Among all cases of GBS early-onset-disease, 72% occur in term newborns (9). However, rates of mortality and morbidity related to GBS early-onset-disease are markedly higher among preterm newborns (mortality 19.2% vs. 2.1% respectively). Preterm neonates with GBS early-onset-disease are more likely to experience apnea, require blood pressure support, and need neonatal intensive care (10).
Risk Factors Associated with GBS Early-Onset-Disease
The primary risk factor for neonatal GBS early-onset-disease is maternal vaginal-rectal colonization with GBS during the intrapartum period. Other risk factors include gestational age less than 37 weeks, very low birth weight, prolonged rupture of membranes, intraamniotic infection, young maternal age, and maternal black race (11). Heavy vaginal-rectal colonization, GBS bacteriuria, and having a previous newborn affected by GBS early-onset-disease also are associated with an increased risk (12). During any trimester, GBS isolated in clean catch urine specimens at any colony count is considered a surrogate for heavy-rectal colonization.
Universal Antepartum Screening
The CDC first recommended universal antepartum culture-based screening of all pregnant women in the 2002 perinatal GBS guidelines, and universal antepartum culture-based screening continues to be the current standard (13). Regardless of planned mode of birth, all pregnant women should undergo antepartum screening for GBS at 36 0/7 – 37 6/7 weeks of gestation, unless intrapartum antibiotic prophylaxis for GBS is indicated because of GBS bacteriuria during the pregnancy or because of a history of a previous GBS-infected newborn.
The 2010 version of the CDC’s perinatal GBS guidelines recommended that prenatal GBS screening be performed starting at 35 0/7 weeks of gestation. The ACOG now recommends performing universal GBS screening between 36 0/7 and 37 6/7 weeks of gestation. The rationale for changing the timing of universal GBS screening is based on two factors:
- The use of antibiotic prophylaxis is recommended as a default for women with unknown GBS screening test results who give birth before 37 0/7 weeks of gestation.
- This new recommended timing for screening provides a 5-week window for valid culture results that include births that occur up to the gestational age of at least 41 0/7 weeks. In the United States, 1.9% of women give birth between 35 0/7 and 35 6/7 weeks gestation versus 6.7% who give birth at 41 0/7 weeks of gestation or more (14).
This change is also likely to reduce the reported incidence of discrepant antepartum culture results and colonization status at the time of birth. In clinical situations in which a pregnant women at term does not give birth within this 5-week screening accuracy window, and whose original GBS screening culture was negative, repeat GBS screening is reasonable and may help guide management beyond 41 0/7 weeks of gestation.
Collection and Culture of Specimen
To maximize the likelihood of GBS recovery, a single swab is used to obtain the culture specimen first from the lower vagina (near the introitus) and then from the rectum (through the anal sphincter) without use of a speculum. Place the swab(s) into a nonnutritive transport medium (e.g., Stuart or Amines medium with or without charcoal). GBS isolates can remain viable in transport media for several days at room temperature; however, the recovery of isolates declines within 1-4 days, especially at elevated temperatures, which can lead to false-negative test results (15).
- Specimen requisitions should clearly indicate that specimens are for GBS culture obtained from a pregnant woman. If woman reports an allergy to penicillin, the laboratory requisition that accompanies the screening GBS culture should be marked for the laboratory to ensure that appropriate testing of any GBS isolates for susceptibility is performed. If a woman is determined to be at high risk of anaphylaxis to penicillin, susceptibility testing for clindamycin should be ordered.
- Laboratories should process sample swabs identified as intended for GBS culture by incubating first in appropriate selective enrichment broth to optimize sensitivity of subsequent culture results.
- After incubation in enrichment broth, a subculture is made onto blood agar plates, followed by identification of any bacterial colonies as GBS using latex agglutination with group B antisera, chromogenic agars, DNA probes, or nucleic acid amplification tests.
- Inducible resistance to clindamycin is detected by the D-zone test, which tests the isolate for resistance to clindamycin.
A key step in this process is incubation of the specimen in enrichment broth before inoculation onto agar culture plates. This method has been shown to maximize GBS identification in culture (16).
Molecular-Based (Nucleic Acid) Testing for GBS
Currently, culture-based testing remains the standard for maternal antepartum GBS screening. The laboratory may also use direct latex agglutination tests of nucleic acid amplification testing (NAAT) on the enriched selective broth as an additional or alternative method for processing of antepartum cultures. Rates for GBS detection using NAAT methods have been shown to be equivalent to culture-based screening or better when the test protocol includes and 18 – 24-hour incubation step in enrichment broth before performing the NAAT analysis, which is similar to the process for traditional culture-based methods. Therefore, NAAT-based testing offers a reasonable and potentially more sensitive alternative to a culture for antepartum screening and some laboratories, albeit a minority, report the use of these newer tests for routine antepartum screening (17).
NAAT methods for GBS detection also can be used for intrapartum management as a rapid test performed at the time of presentation in labor or for women at term who have unknown or unavailable antepartum GBS screening test results. However, although a 1-2-hour turnaround time is reported when NAAT is uses as a point-of-care test, this time advantage does not allow for the full enrichment broth incubation step that is needed to maximize results. At present, an approach consisting of NAAT-based intrapartum testing alone has not been shown to adequately replace routine prenatal screening at 36 0/7 – 37 6/7 weeks of gestation (18).
Indication for Intrapartum Antibiotic Prophylaxis
Exception to universal prenatal GBS vaginal-rectal culture are women who have GBS bacteriuria identified at any time during the current pregnancy and those who have previously given birth to a neonate with GBS early-onset-disease because these risk factors are overriding indications for intrapartum antibiotic prophylaxis (19). See table 1 below
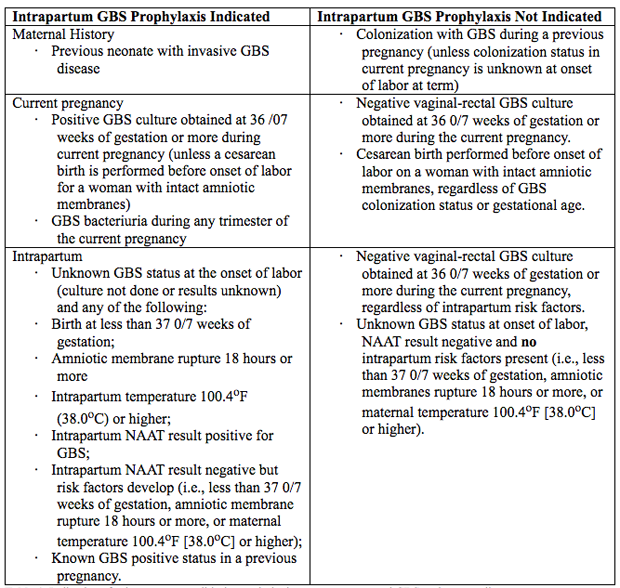
Table 1. Indications for intrapartum antibiotic prophylaxis to prevent neonatal GBS early-onset-disease.
Abbreviations: GBS: group B streptococcus; NAAT: nucleic acid amplification test.
Bacteriuria
Intrapartum antibiotic prophylaxis indications are:
- GBS bacteriuria at any concentration identified at any time in pregnancy represents heavy maternal vaginal-rectal colonization and indicates the need for intrapartum antibiotic prophylaxis, without the need for a subsequent GBS screening vaginal-rectal culture at 36 0/7 – 37 6/7 weeks of gestation (20).
- GBS bacteriuria at levels of 105 CFU/mL or greater, with asymptomatic or symptomatic, warrants acute treatment and indicates the need for intrapartum antibiotic prophylaxis at the time of birth.
- Identification of asymptomatic bacteriuria with GBS during pregnancy at a level less than 105 CFU/mL does not require maternal antibiotics therapy during the antepartum period but it is an indication for intrapartum antibiotic prophylaxis at the time of birth (21).
- A urine culture sent for laboratory evaluation during pregnancy for any indication should be marked as being that of a pregnant woman.
- In woman who have reported penicillin allergy, the laboratory requisition that accompanies an antepartum urine culture should be specifically marked for the laboratory to be aware of the penicillin allergy, to ensure that any GBS isolate identified will be appropriately tested for clindamycin susceptibility.
- Clindamycin susceptibility results reported on an antepartum GBS-positive urine culture are ONLY for the purpose of guiding the choice of antibiotic for intrapartum antibiotic prophylaxis during labor. If antepartum treatment or a urinary tract infection or bacteriuria is indicated, clindamycin is not recommended as a treatment agent, even in women allergic to penicillin. It is concentrated poorly in urine, metabolized primarily by the liver, and is intended to treat bloodstream and soft tissue, not urinary infections.
Preterm Labor
An algorithm for management of women with preterm labor is outlined in Figure 2. Intrapartum prophylaxis for GBS should be started while initial management of possible preterm labor is being undertaken. If preterm labor progresses, intrapartum, antibiotic prophylaxis for GBS should be continued during labor.
- If preterm birth is determined not to be imminent, intrapartum antibiotic prophylaxis for GBS can be stopped and subsequent management can be guided by the most recent culture result.
- If the preterm GBS cultures was positive, the culture does not need to be repeated, and intrapartum antibiotic prophylaxis for GBS should be reinstituted whenever labor occurs (22).
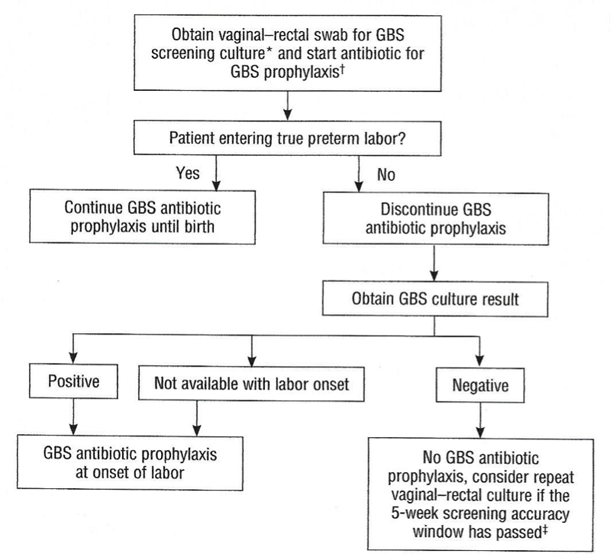
Figure 2. Management of women with preterm labor <37 0/7 weeks of gestation.
Abbreviation: GBS, group B streptococcus.
*If a patient has undergone vaginal-rectal GBS screening culture within the preceding 5 weeks, the results of that culture should guide management.
†See details below for recommended antibiotic management.
‡A negative GBS culture is considered valid for 5 weeks.
- If the GBS culture result is unavailable and preterm labor reoccurs, then intrapartum antibiotic prophylaxis should be reinstituted. If a GBS culture was not obtained previously, then a new GBS culture should be obtained before restarting antibiotics.
- If the GBS culture was negative and preterm reoccurs within 5 weeks, intrapartum antibiotic prophylaxis for GBS prophylaxis is not necessary.
- If the patient remains pregnant for 5 or more weeks after a negative baseline GBS test, then GBS screening should be repeated if a recurrent episode of preterm labor occurs at or 36 0/7 – 37 6/7 weeks of gestation.
Preterm Prelabor Rupture of Membranes (PPROM)
An algorithm for the management of women with PPROM is outlined in Figure 3. Current ACOG guidelines recommend proceeding to delivery if PPROM occurs at or beyond 34 0/7 weeks of gestation (23).
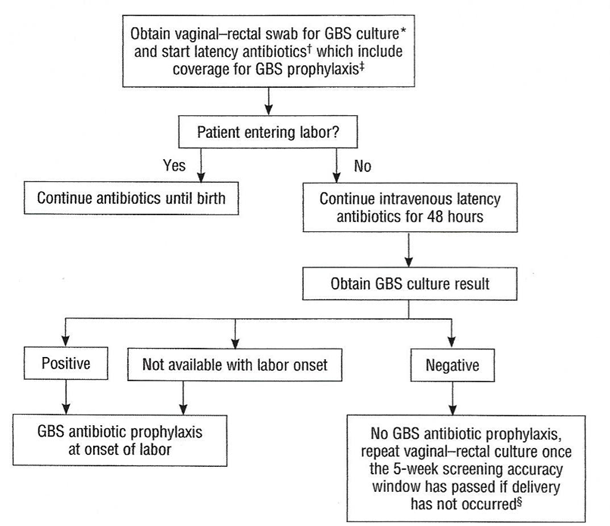
Figure 3. Management of women with Preterm Prelabor Rupture of Membranes (PPROM).
Abbreviation: GBS, group B streptococcus.
*If a patient has undergone vaginal-rectal GBS culture within the preceding 5 weeks, the results of that culture should guide management.
†Latency antibiotics that include ampicillin given in the setting of PPROM are adequate for GBS prophylaxis.
‡See details below for recommended antibiotic regimens.
§A negative GBS culture is considered valid for 5 weeks. However, the number of weeks is based on early-term screening and data in preterm gestation is lacking.
If a patient with PPROM is entering labor and had a negative GBS culture more than 5 weeks previously, she should be rescreened and managed according to this algorithm (see figure 3) at that time. Two secondary analyses of large multicenter randomized controlled trials of PPROM in women colonized with GBS found a lower risk of neonatal infect associated with immediate induction in women who were later preterm (34 0/7 – 36 6/7 weeks of gestation) and early term (37 0/7 – 38 6/7 weeks of gestation) (24). In such cases, immediate induction rather than extended expectant management is recommended.
Planned Cesarean Birth
Intrapartum prophylaxis that is specific for GBS is not recommended for women undergoing a planned cesarean birth in the absence of labor and PPROM, regardless of the gestation age, even among women who are GBS positive. Multistate surveillance reveals that GBS early-onset-disease occurs at a very low rate in this situation, approximately 3 per 1,000,000 live births (24). This does not change the recommendation that women undergo cesarean birth (regardless of GBS colonization status) be administered one dose of prophylactic antibiotics before the incision to reduce the risk of postoperative infections (22).
Women planning cesarean birth should nonetheless undergo prenatal GBS culture at 36 0/7 - 36 6/7 weeks of gestation because onset of labor or PPROM may occur before the planned cesarean birth. Should a woman with a planned cesarean birth and a positive antepartum GBS culture present in active labor or with PPROM before her scheduled delivery date, a single dose of an antibiotic (or combination of antibiotics) that provides GBS prophylaxis and presurgical prophylaxis is appropriate. In most clinical situations, cefazolin will meet both these criteria. Delaying the cesarean birth to administer additional doses of antibiotics for GBS prophylaxis alone is not indicated.
Unknown Culture Status During Labor at Term
There are three ways to identify candidates for intrapartum antibiotic prophylaxis when a woman at term presents in labor with unknown GBS culture status and does not have an established indication for intrapartum antibiotic prophylaxis. In this situation:
- The intrapartum use of maternal risk factors;
- Molecular-based testing (e.g., nucleic acid amplification test); or
- Known history of GBS colonization in a previous pregnancy may be used.
When a woman is in labor and her GBS colonization status is unknown, a temperature of 100.4oF (38oC) or higher, or rupture of membranes for 18 hours or more, is independently associated with an increased risk of neonatal GBS early-onset-disease (25). Although reduction of neonatal prophylaxis, if suspected or confirmed intraamniotic infection develops, intrapartum antibiotic prophylaxis targeted against GBS should be converted to a more broad-spectrum antibiotic regimen for treatment of intraamniotic infection that includes activity against GBS, generally ampicillin and an aminoglycoside (26).
Intrapartum Antibiotic Prophylaxis
Intrapartum antibiotic prophylaxis to reduce the risk of GBS early-onset-disease is based on a two-pronged approach:
- Decreasing the incidence of neonatal GBS colonization, which requires adequate maternal drug levels, and
- Reducing the risk of neonatal sepsis, which requires adequate antibiotic levels in the fetus and newborn.
Antimicrobial Agents
Intravenous penicillin remains the agent of choice for intrapartum prophylaxis, with intravenous (IV) ampicillin as an acceptable alternative. Penicillin is the preferred first-line agent because it has a narrow, more targeted spectrum of antimicrobial activity against gram-positive bacteria and lower likelihood of inducing resistance in other vaginal organisms. The current recommendations are (27):
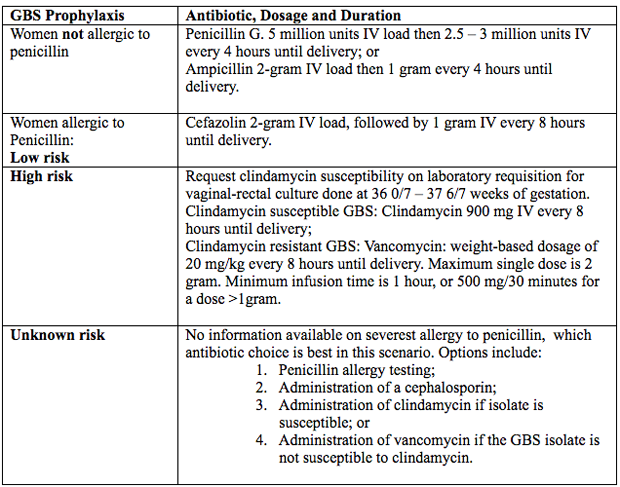
Figure 4. Intrapartum antibiotic prophylaxis. Abbreviations: GBS (group B streptococcus); IV (intravenous)
Penicillin Allergy in Pregnancy
Penicillin was first used almost 80 years ago in 1941, to successfully treat a person with a life-threatening streptococcal infection. Over the remainder of the 20th century, advances in antibiotic therapy led to a decrease in infections as the cause of mortality in the United States from, 33% to 4.5% in 1999 (28). In obstetrics and gynecology, these classes of antibiotics are commonly used to treat urinary tract, intrapartum, postpartum and sexually transmitted infections. One of the most common uses of these antimicrobial agents is intrapartum prophylaxis for GBS colonization. Penicillin allergies has led to routine use of alternative but potentially less effective agents. Individuals treated with alternative antibiotic regimens in the setting of a presumed penicillin allergy have also been shown to have longer-duration hospitalizations (29). Furthermore, broad-spectrum antibiotics are often more costly. A specific and common example of this problem in obstetrics is the need to incorporate alternative penicillin-antibiotic regimens for intrapartum antibiotic prophylaxis against neonatal GBS early-onset-disease owning to a reported, frequently undocumented, maternal history of penicillin allergy.
Importantly, most individuals who report a penicillin allergy are neither truly allergic nor at risk of a developing a hypersensitivity reaction after exposure to penicillin. Approximately 80 – 90% of persons with a history penicillin allergy are actually penicillin tolerant (29). There are a number of reasons for this seeming contradiction. First, the risk of recurrence for even IgE-mediated penicillin reaction has been shown to dissipate over time. It has been reported that elicitable sensitivity to penicillin is no longer present by 5 years after a reported IgE-mediated reaction in approximately 50% of individuals, and this rate increases to at least 80% by 10 years after the reaction (30). Thus, many adults today have a history of penicillin allergy that does not represent a risk for true recurring penicillin hypersensitivity that would preclude its subsequent use. In addition, a common confounding scenario that can result in a presumed penicillin allergy occurs when the original adverse reaction was not directly related to penicillin.
Evaluation of Penicillin Allergy
Questions and interpretation of answers below, can help determine the probability that the allergic reaction was an IgE-mediated hypersensitivity reaction or rare severe form of T-cell response (31).
- How long did this reaction occur? IgE-mediated reactions disappear over time, with approximately 80% of persons no longer reactive after 10 years.
- What symptoms did you have when the allergic reaction occurred? Reactions such as delayed maculopapular rash and gastrointestinal upset are not likely to be secondary to an IgE-mediated hypersensitivity reaction. If the history includes angioedema, hives, anaphylaxis, bronchospasm, or rare delayed reactions such as Stevens-Johnson syndrome, the allergic reaction is likely high-risk for recurrence.
- When did the symptoms occur? Symptoms occurring immediately after exposure are more likely to be high-risk for anaphylaxis than are symptoms that develop several hours or days after exposure.
- How was the reaction treated? If symptoms cannot be re-called, it can help to determine whether the treatment included hospitalization or care in an emergency department.
- Have you had the same symptoms more than once after receiving an antibiotic? Persons who have recurrent reactions to antibiotics are more likely to have high-risk allergy.
- Have you been given penicillin, ampicillin, or another type or penicillin since you had this reaction? If the individual has received any form of penicillin without recurrent reaction, the allergy is likely low-risk.
Definitions of Penicillin Allergy
The determination of risk is further confounded by a lack of standard classifications or terminology among national medical societies and individual experts to facilitate distinguishing allergy risk categories. In addition, there are no universally recommended allergy history questionnaires to assist with clinical assessment, though several have been evaluated in published research in attempts to validate their effectiveness as components of penicillin allergy evaluation guidelines. The following definitions are recommended by ACOG (19).
Low Risk:
Nonspecific symptoms unlikely to be allergic – gastrointestinal distress, headaches, yeast vaginitis.
Non-urticarial maculopapular (morbilliform) rash without systemic symptoms. This rash typically occurs several days after initial exposure and is limited to the skin (mucus membrane, palms and soles are not involved). May be mildly pruritic, but not urticarial.
Pruritis without rash.
Family history of penicillin allergy but no personal history.
Patient reports history but has no recollection of symptoms or treatment.
High Risk:
High risk for anaphylaxis: A history suggestive of an IgE-mediated event (anaphylactic reactions are IgE-mediated and typically occur within 1-6 hours after exposure to a penicillin), pruritic rash, urticaria (hives), immediate flushing, hypotension, angioedema, respiratory distress or anaphylaxis.
Recurrent reactions, reactions to multiple beta-lactam antibiotics, or positive penicillin allergy test.
High risk for severe IgE-mediated reaction: Severe rare delayed-onset cutaneous or systemic reactions, such as eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome, Stevens-Johnson syndrome, or toxic epidermal necrolysis.
Severe rare delayed-onset reactions, such as eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome, Stevens-Johnson syndrome, or toxic epidermal necrolysis are T-cell mediated and typically occur days to weeks after initiation of antibiotic treatment. Some experts consider these a contraindication to standard penicillin allergy.
Penicillin Allergy Testing
Formal targeted drug allergy testing assessments can confer real benefit to patients, either to substantiate the reported adverse drug reaction, especially when the historical recollection of allergy is unclear, or to exclude it. Penicillin allergy testing has been shown to be safe to perform and can be beneficial for all women who report a penicillin allergy, particularly those whose symptom descriptions are suggestive of being IgE-mediated, of unknown severity, or both. Pregnancy presents a unique challenge owing to both maternal and provider concerns that the allergy evaluation itself may have an untoward effect not only on the woman but on her fetus as well. Two small studies have described the safety and performance of penicillin skin testing in pregnant women who reported a penicillin allergy and were subsequently screened as positive GBS colonization in the 3rd trimester. Between 93% to 96% of these women underwent successful outpatient penicillin allergy skin testing without any complications and subsequently were able to receive penicillin as intrapartum antibiotic prophylaxis for their GBS colonization (32).
More recent consensus guidelines advocate for pregnant women with allergy histories and negative penicillin skin allergy testing to have follow-up confirmation with an oral amoxicillin challenge (33). In locations without access to skin-testing materials, an oral amoxicillin challenge test only (without skin-testing initially) for low-risk patients has been recommended (33). The logistics of a protocol for testing in pregnancy include: a requirement that the clinical sites be staffed by the necessary personnel (such as physicians, pharmacists, and nurses trained in penicillin allergy testing), that required materials for the penicillin skin testing be available on site, and that management protocols be in place, with appropriate medications readily available, in the uncommon event of a drug challenge reaction. This may require the testing to be performed in a setting that can accommodate a short length of stay (several hours) and continued monitoring of both the woman and her fetus during the testing process, depending on gestational age.
Maternal Obesity and Cord Blood Penicillin Levels
It has been shown in other clinical scenarios that higher antibiotic doses are required to achieve adequate therapeutic effects in patients with obesity. Both pregnancy and obesity can alter the pharmaco-kinetics and pharmaco-dynamics of many medications, and β-lactam antibiotics have been shown to have and increased volume of distribution in patients with obesity (34). This increased volume of distribution can lead to diminished therapeutic benefit at the relevant tissue. Maternal obesity is a known risk factor for neonatal GBS disease, though this risk has generally been attributed to higher rates of GBS colonization among women with obesity. However, these data raise the question of whether the recommended intrapartum antibiotic prophylaxis dose could possibly be inadequate in women with obesity.
There are limited data about the pharmaco-kinetics of penicillin in women in the third trimester of pregnancy, especially in the setting of obesity. No data exist to confirm that the standard dosing of penicillin for intrapartum prophylaxis achieves adequate therapeutic concentration in patients with obesity.
This prospective cohort study (35), of term women receiving intrapartum penicillin prophylaxis for GBS colonization (determined by antenatal rectovaginal culture). The following outcomes were compared between obese (body mass index [BMI] 35 or higher at delivery) and non-obese (BMI less than 30 at delivery) groups: penicillin concentration in maternal blood (after two penicillin doses) and umbilical cord blood, GBS rectovaginal colonization status on admission and after two completed doses, and neonatal GBS colonization (using a postnatal ear swab). 55 women were needed to detect a 0.75 SD difference in cord blood penicillin concentration. Conclusion: the median cord blood penicillin concentration was 60% lower in neonates born to women with obesity. However, all concentrations exceeded the minimum inhibitory concentration. Maternal penicillin levels were not significantly different between groups. More than 40% of women who previously tested positive for GBS by antenatal culture tested negative for GBS on admission for delivery (35).
Continued research is needed to better understand optimal medication dosing in pregnant women with obesity, and to ensure that the GBS screening and intrapartum antibiotic prophylaxis protocols are as precise and effective as possible.
Recommendations and Key Points
- Targeted intravenous (IV) intrapartum antibiotic prophylaxis has demonstrated efficacy for prevention of GBS early-onset-disease in neonates born to women with positive antepartum GBS cultures and women who have other risk factors for intrapartum GBS colonization. Neither antepartum nor intrapartum oral or intramuscular regimens have been shown to be comparably effective in reducing GBS early-onset-disease.
- Regardless of planned mode of birth, all pregnant women should undergo antepartum screening for GBS at 36 0/7-37 6/7 weeks of gestation, unless intrapartum antibiotic prophylaxis for GBS is indicated because of GBS bacteriuria during the pregnancy or because of a history of a previous GBS-infected newborn. This new recommended timing for screening provides a 5-week window for valid culture results that includes birth that occur up to a gestational age of at least 41 0/7 weeks.
- All women whose vaginal-rectal cultures at 36 0/7 – 37 6/7 weeks of gestation are positive for GBS should receive appropriate intrapartum antibiotic prophylaxis unless a prelabor cesarean birth is performed in the setting of intact membranes.
- Women with a positive prenatal GBS culture result who undergo a cesarean birth before the onset of labor and with intact membranes do not require GBS antibiotic prophylaxis.
- If the prenatal GBS culture result is unknown when labor starts, intrapartum antibiotic prophylaxis is indicated for women who have risk factors for GBS early-onset-disease. At-risk women include those who present in labor with a substantial risk of preterm birth, who have PPROM or rupture of membranes for 18 or more hours at term, or who present with intrapartum fever (temperature 100.4oF [38oC] or higher). If intraamniotic infection is suspected, broad-spectrum antibiotic therapy that provides coverage for poly-microbial infections as well as GBS should replace the antibiotic that provides coverage for GBS prophylaxis specifically.
- If a woman presents in labor at term with unknown GBS colonization status and does not have risk factors that are an indication for intrapartum antibiotic prophylaxis but reports a known history of GBS colonization in a previous pregnancy, the risk of GBS early-onset-disease in the neonate is likely to be increased. With this increased risk, it is reasonable to offer intrapartum antibiotic prophylaxis based on the woman’s history of colonization. Health care providers also may consider discussing the option of empiric intrapartum antibiotic prophylaxis as a shared decision-making process in this clinical scenario.
- Intravenous (IV) penicillin remains the agent of choice for intrapartum prophylaxis, with IV ampicillin as an acceptable alternative. First-generation cephalosporins (i.e., cefazolin) are recommended for women whose reported penicillin allergy indicates a low risk for anaphylaxis or is of uncertain severity. For women with a high risk of anaphylaxis, clindamycin is the recommended alternative to penicillin only if the GBS isolate is known to be susceptible to clindamycin.
- Alternatively, penicillin allergy testing, if available, is safe during pregnancy and can be beneficial for all women who report a penicillin allergy, particularly those that are suggestive of being IgE-mediated, or of unknown severity, or both. Ascertaining the absence of a type I hypersensitivity reaction will eliminate the need to use alternatives to penicillin for GBS early-onset-disease prophylaxis and provide long-term benefit if treatment with beta-lactam antibiotics is indicated in their future healthcare management. Because most women who have a reported penicillin allergy are, in fact, penicillin tolerant, use of penicillin allergy testing is increasingly being used in all areas of healthcare as part of antibiotic stewardship initiatives, and expansion of its use is encouraged in obstetric patients.
- For women who are at high-risk of anaphylaxis after exposure to penicillin, the laboratory requisitions for ordering antepartum GBS screening cultures (whether on paper or online in electronic medical records) should clearly indicate the presence of penicillin allergy. This step is intended to ensure that the need to test GBS isolates for clindamycin susceptibility is recognized and performed by laboratory personnel, and that the healthcare provider understands the importance of reviewing such a test result.
- IV vancomycin remains the only pharmacokinetically and microbiologically validated option for intrapartum antibiotic prophylaxis in women who report a high-risk penicillin allergy and whose GBS isolate is not susceptible to clindamycin. The vancomycin dosage for intrapartum GBS prophylaxis should be based on weight and baseline renal function (20 mg/kg IV every 8 hours, with a maximum of 2 g. per single dose).
- Obstetric interventions, when necessary, should not be delayed solely to provide 4 hours of antibiotic administration before birth. Such interventions include but are not limited to administration of oxytocin, artificial rupture of membranes, or planned cesarean birth, with or without pre-cesarean rupture of membranes. However, some variation in practice may be warranted based on the needs of individual patients to enhance intrapartum antibiotic exposure.
Breastfeeding
Breastfeeding shapes the neonatal gut microbiota, both because of exposure to the milk microbiota and via factors such as milk oligosaccharides, secretory IgA and antimicrobial antibodies, which are thought to guide the infants’ developing mucosal immune system (36). There has been a concern that some cases of the late-onset GBS disease are secondary to transmission via the mother’s milk, but in other cases the immune factors in breast milk may be protective. One small study has suggested that, results demonstrate the benefit of continued breastfeeding after emergency cesarean section, in promoting a positive-weaning gut microbiota profile comparable to vaginally born infants without intrapartum antibiotic prophylaxis, but no such ameliorating effect was seen with babies born vaginally (36). Any effect of breast feeding on the microbiota following intrapartum needs further study.
Summary
Universal prenatal, culture-based screening for maternal GBS colonization and intrapartum antibiotic prophylaxis together currently constitutes the most effective strategy for reducing perinatal morbidity and mortality secondary to GBS. To date, this regimen has been associated with a significant decrease in the incidence of GBS early-onset-disease and has not been associated with adverse effects in women or newborns. Intrapartum screening using NAAT for GBS has been shown to have high sensitivity and specificity, but many of these tests need several hours of enrichment to attain that level of performance, which limits their value if a result is needed rapidly. Appropriate collection of vaginal-rectal GBS screening cultures, proper use of indicated antibiotics, and optimization of the correct application of intrapartum antibiotic prophylaxis, along with educational efforts to reinforce understanding of those practices, are key to minimizing the risk of GBS early-onset-disease.
As many as 30% of pregnant women will receive some type of antibiotic therapy over the course of pregnancy, labor and birth, with penicillin being the most prescribed antibiotic used for antepartum and intrapartum prophylaxis in women who have screened positive during pregnancy for GBS colonization. Still, reported penicillin allergies prevent women from receiving this first-line-narrow-spectrum antibiotic when indicated, while they may have implications for prevention of neonatal infection. antibiotic stewardship initiatives designed to focus, limit and guide the use of these potent but fragile pharmacologic agents in practice are a critical component of optimizing care across all health care facilities. The long-term benefits of evaluating penicillin allergy, especially prenatally, include the ability to use the first-line antimicrobial agents proven to be most effective when needed, as well as the possibility of lowering the rates of complications related to both infections and their treatments. We advocate for wider consideration and adoption of penicillin allergy testing in pregnant women specifically and the female population in general.
Suggested Reading
Group B Streptococcal Perinatal Infection: A Comprehensive Review
http://www.womenshealthsection.com/content/obsidp/obsidp006.php3
References
- Baltimore RS, Huie SM, Meek JI, et al. Early-onset sepsis in the era of group B streptococcal prevention. Pediatrics 2001;108(5):1094-1098
- Shabayek S, Spellerberg B. Group B streptococcal colonization, molecular characteristics, and epidemiology. Front Microbiol 2018;9:437
- Tsai MH, Hsu JF, Lai MY, Lin LC, et al. Molecular characteristics and antimicrobial resistance of group B Streptococcus strains causing invasive disease in neonates and adults. Front Microbial 2019;10:264
- Nanduri SA, Petit D, Smelser C, Aposol M, et al. Epidemiology of invasive early-onset and late-onset group B streptococcal disease in the United States, 2006 to 2015: multistate laboratory and population-based surveillance [preprint]. JAMA Pediatr 2019. DOI: 10.1001/jamaperidatrics.2018.4826
- Bianchi-Jassir F, Seale AC, Kohli-Lynch M, et al. Preterm birth associated with group B streptococcus maternal colonization worldwide: systematic review and meta-analyses. Clin Infect Dis 2017;65:S133-S142
- Le Doare K, Heath PT. An overview of global GBS epidemiology. Vaccine 2013;31(suppl 4):D7-D12
- Berardi A, Rossi C, Lugli L, Creti R, et al. Group B streptococcus late-onset disease; 2003-2010. GBS Prevention Working Group, Emilia-Romanga. Pediatrics 2013;131:e361-e368
- Russell NJ, Seale AC, O’Sullivan C, et al. Risk of early-onset neonatal group B streptococcal disease with maternal colonization worldwide: systemic review and meta-analyses. Clin Infect Dis 2017;65:S152-S159
- Creti R, Imperi M, Beradi A, et al. Neonatal group B streptococcus infections: prevention strategies, clinical and microbiologic characteristics in 7 years of surveillance. Italian Neonatal GBS Infections Working Group. Pediatr Infect Dis 2017;36:256-262
- Stoll BJ, Hansen NI, Sanchez PJ, et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Pediatrics 2011;127:817-826
- Puopolo KM, Draper D, Wi S, Newman TB, et al. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics 2011;128:e1155-e1163
- Kessous R, Weintraub AY, Sergienko R, Lazer T, et al. Bacteriuria with group B streptococcus: is it a risk factor for adverse pregnancy outcome? J Matern Fetal Neonatal Med 2012;25:1983-1986
- Schrag S. Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep 2002;51:1-22
- Martin JA, Osterman MJ, Kirmeyer SE, Gregory EC. Measuring gestational age in vital statistics data: transitioning to the obstetric estimate. Natl Vital Stat Rep 2015;64:1-20
- Verani JR, Spina NL, Lynfield R, Schaffner W, et al. Early-onset group B streptococcal disease in the United States: potential for further reduction. Obstet Gynecol 2014;123:828-837
- Church DL, Baxter H, Lloyd T, Miller B, Elsayed S. Evaluation of Strep B carrot broth versus Lim broth for detection of group B Streptococcus colonization status of near-term pregnant women. J Clin Microbiol 2008;46:2780-2782
- Fay K, Almendrares O, Robinson-Dunn B, Scharg S. Antenatal and intrapartum nucleic acid amplification test use for group B streptococcus screening – United States, 2016 [preprint]. Diagn Microbiol Infect Dis 2018. DOI: 10.1016/j.diagmicrobio.2018.11.026
- Couturier BA, Weight T, Elmer H, Schlaberg R. Antepartum screening for group B streptococcus by three FDA-cleared molecular tests and effect of shortened enrichment culture on molecular detection tests. J Clin Microbiol 2014;52:3429-3432
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 797. Prevention of group B Streptococcal early-onset disease in newborn. Obstet Gynecol 2020;135:e51-e72
- Perez-Moreno MO, Pico-Plana E, Grande-Armas J, et al. Group B streptococcal bacteriuria during pregnancy as a risk factor for maternal intrapartum colonization: a prospective cohort study. J med Microbiol 2017;66:454-460
- Allen VM, Yudin MH. 276-management of group B streptococcal bacteriuria in pregnancy. J Obstet Gynecol Can 2018;40:e181-e186
- American College of Obstetricians and Gynecologists. Use of prophylactic antibiotics in labor and delivery. ACOG Practice Bulletin No. 199. Obstet Gynecol 2018;132:e103-e119
- American College of Obstetricians and Gynecologists. Prelabor rupture of membranes. ACOG Practice Bulletin No. 188. Obstet Gynecol 2018;131:e1-e14
- Tajik P, van der Ham DP, Zafarmand MH, Hof MH, et al. Using vaginal group B streptococcus colonization in women with preterm premature rupture of membranes to guide the decision for immediate delivery: a secondary analysis of the PPROMEXIL trials. BJOG 2014;121:1263-1272
- Lin FY, Brenner RA, Johnson YR, Azimi PH, et al. The effectiveness of risk-based intrapartum chemoprophylaxis for the prevention of early-onset neonatal B streptococcal disease. Am J Obstet Gynecol 2001;184:1204-1210
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 712. Intrapartum management of intraamniotic infection. Obstet Gynecol 2017;130:e95-e101
- Verani JR, McGee L, Schrag SJ. Prevention of perinatal group B streptococcal disease: revised guidelines from CDC, 2010. Division of Bacterial Diseases. National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). MMWR Recomm Rep 2010;59(RR-10):1-36
- Ligon BL. Penicillin: its discovery and early development. Semin Pediatr Dis 2004;15:52-57
- Macy E, Conteras R. Health care use and serious infection prevalence associated with penicillin “allergy” in hospitalized patients: a cohort study. J Allergy Clin Immunol 2014;133:790-796
- Trubiano JA, Adkinson NF, Phillips EJ. Penicillin allergy is not necessarily forever. JAMA 2017;318:82-83
- Gonzalez-Estrada A, Radoicic C. Penicillin-allergy: a practical guide for clinicians. Cleveland Clin J Med 2015;82:295-300
- Philpson EH, Lang DM, Gordon SJ, et al. Management of group B streptococcus in pregnant women with penicillin allergy. J Reprod Med 2007;52:480-484
- Turrentine MA, King TL, Silverman NS. Penicillin allergy in pregnancy: moving from “rash” decisions to accurate diagnosis. Obstet Gynecol 2020;135:401-408
- Meng L, Mui E, Holubar Mk, Deresinski SC. Comprehensive guidance for antibiotic dosing in obese adults. Pharmacotherapy 2017;37:1415-1431
- McCoy JA, Elovitz MA, Alby K, et al. Association of obesity with maternal and cord blood penicillin levels in women with group B streptococcus colonization. Obstet Gynecol 2020;136:756-764
- Steer PJ, Russell AB, Kochhar D, Cox P, et al. Group B streptococcal disease in the mother and newborn: a review. Eu J Obstet Gynecol Reprod Biol 2020;252:526-533
Publicado: 4 February 2021
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


