Newborn Hearing Loss Detection and Intervention
WHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC).
Hearing loss can affect a child’s ability to develop communication, language, and social skills. The earlier children with hearing loss start getting services, the more likely they are to reach their full potential. If you are a parent and you suspect your child has hearing loss, trust your instincts and speak with your child’s doctor. Most children hear and listen to sounds at birth. They learn to talk by imitating the sounds they hear around them and the voices of their parents and caregivers. But that is not true for all children. In fact, about 2 or 3 out of every 1,000 children in the United States (US) are born with detectable hearing loss in one or both ears. More lose hearing later during childhood. Children who have hearing loss may not learn speech and language as well as children who can hear. For this reason, it is important to detect deafness or hearing loss as early as possible. Because of the need for prompt identification for childhood hearing loss, universal newborn hearing screening programs currently operate in all U.S. states and most U.S. territories. With help from the federal government, every state has established an Early Hearing Detection and Intervention Program. As a result, more than 96% of babies heave their hearing screened within 1 month of birth.
The purpose of this document is to review the importance of baby’s hearing screening, how it is done and the types of intervention services available. The most important time for a child to learn language is in the first 3 years of life, when the brain is developing and maturing. In fact, children begin learning speech and language in the first 6 months of life. Research suggests that children with hearing loss who get help early develop better language skills than those who do not.
Introduction
A hearing loss can happen when any part of the ear is not working in the usual way. This includes the outer ear, middle ear, inner ear, hearing (acoustic) nerve, and auditory system. The acoustic nerve sends sound information from ear to the brain and the auditory system processes sound information as it travels from the ear to the brain.
According to the Centers for Disease Control and Prevention (CDC), currently around 98% of newborns are screened for hearing loss in the US, annually. Since more than 50,000 infants who are deaf and hard-of-hearing have been identified within the first year of life and have had the opportunity to receive early intervention services that can help them reach their full potential.
Before 1993, fewer than 1 in 10 newborns in the US, were screened for hearing loss, but now nearly all are screened. According to CDC in 2017 (1):
- 95.5% of all infants were screened prior to one month of age, and overall, 98.2% of all infants born in the US have their hearing screened.
- 58.7% of infants received audiological evaluations and a diagnosis by three months of age. Our system continues to work to increase the number of infants identified as deaf or hard-of-hearing, at an early age. In 2015, 279 more infants were identified from the previous year, for a total of 6,442 infants identified as deaf or hard-of-hearing.
- 65.3% of infants were enrolled in early intervention services before six months of age.
Definitions
The functions, skills and abilities of voice, speech, and language are related. Some dictionaries and textbooks use the terms almost interchangeably. But for scientists and medical professionals, it is important to distinguish among them.
Voice (or Vocalization): It is the sound produced by humans and other vertebrates using the lungs and the vocal folds in the larynx, or voice box. Voice is not always produced as speech, however. Infants babble and coo; animals bark, moo, whinny, growl, and meow; and adult humans laugh, sing and cry. Voice is generated by airflow from the lungs as the vocal folds are brought close together. When air is pushed past the vocal folds with sufficient pressure, the vocal folds vibrate. If the vocal folds in the larynx did not vibrate normally, speech could only be produced as a whisper. Your voice is as unique as your fingerprint. It helps define your personality, mood, and health.
According to the National Institute on Deafness and Other Communication Disorder (NIDCD), approximately, 17.9 million adults in the US have trouble using their voices. Disorders of the voice involve problems with pitch, loudness, and quality. Pitch is the highness or lowness of a sound based on the frequency of the sound waves. Loudness is the perceived volume (or amplitude) of the sound, while quality refers to the character or distinctive attributes of a sound.
Speech: Humans express thoughts, feelings, and ideas orally to one another through a series of complex movements that alter and mold the basic tone created by voice into specific, decodable sounds. Speech is produced by precisely coordinated muscle actions in the head, neck, chest, and abdomen. Speech development is a gradual process that requires years of practice. During this process, a child learns how to regulate these muscles to produce understandable speech.
In the US, roughly 5% of children have noticeable speech disorders, according to NIDCD. The majority of these speech disorders have no known cause. One category of speech disorder is fluency disorder, or stuttering, which is characterized by a disruption in the flow of speech. It includes repetitions of speech sounds, hesitations before and during speaking, and the prolonged emphasis of speech sounds. More than 15 million individuals in the world stutter, most of whom began stuttering at an early age. The majority of speech sound disorders in the preschool years occur in children who are developing normally in all other areas. Speech disorders also may occur in children who have developmental disabilities.
Language: It is the expression of human communication through which knowledge, belief, and behavior can be experienced, explained, and shared. This sharing is based on systematic, conventionally used signs, sounds, gestures, or marks that convey understood meanings within a group or community. Recent research identifies "windows of opportunities" for acquiring language - written, spoken, or signed - that exist within the few years of life.
According to NIDCD, between 6 and 8 million individuals in the US have some form of language impairment. Disorders of language affect children and adults differently. For children who do not use language normally from birth, or who acquire an impairment during childhood, language may not be fully developed or acquired. Language disorders also are found in adults who have failed to develop normal language skills because of mental retardation, autism, hearing impairment, or other congenital or acquired disorders of brain development. Many adults acquire language disorders because of stroke, head injury, dementia, or brain tumors.
Signs and Symptoms of Hearing Loss
The signs and symptoms of hearing loss are different for each child. Even if a child passed a hearing screening before, it is important to look out for the following signs.
Signs in babies: Does not startle at loud noises; Does not turn to the source of a sound after 6 months of age; Does not say single words, such as “dada” or “mama” by 1 year of age; Turns head when he or she sees you but not if you only call out his or her name. This sometimes is mistaken for not paying attention or just ignoring but could be the result of partial or complete hearing loss; Seems to hear some sounds but not others.
Signs in children: Speech is delayed; Speech is not clear; Dose not follow directions. This sometimes is mistaken for not paying attention or just ignoring but could be the result of a partial or complete hearing loss; Often stays “Huh?” and Turns the television volume up too high.
Babies and children should reach milestones in how they play, learn, communicate, and act (2). A delay in any of these milestones could be a sign of hearing loss or other developmental problem. CDC’s Development Milestones – from 2 months to 5 years; available @ https://www.cdc.gov/ncbddd/actearly/pdf/checklists/Checklists-with-Tips_Reader_508.pdf
Screening and Diagnosis of Hearing Loss
Hearing screening is a test to tell if people might have hearing loss. Hearing screening is easy and not painful. In fact, babies are often asleep while being screened. It takes a noticeably short time – usually only a few minutes.
Babies:
- All babies should be screened for hearing loss no later than 1 month of age. It is best if they are screened before leaving the hospital after birth.
- If a baby does not pass a hearing screening, it is particularly important to get a full hearing test as soon as possible, but no later than 3 months of age.
Older Babies and Children
- If you think a child might have hearing loss, ask the doctor for a hearing test as soon as possible.
- Children who are at risk of acquired, progressive, or delayed-onset hearing loss should have at least one hearing test by 2 to 2 ½ years of age. Hearing loss that gets worse over time is known as acquired or progressive hearing loss. Hearing loss that develops after baby is born is called delayed-onset hearing loss.
- If a child does not pass a hearing screening, it is particularly important to get a full hearing test as soon as possible.
Screening Tests
Two different tests are used to screen for hearing loss in babies. Your babies can rest and sleep during both tests.
1. Otoacoustic Emissions (OAE): It tests whether some parts of the ear respond to sound. During this test, a soft earphone is inserted into your baby’s ear canal. It plays sounds and measures an echo response that occurs in ears with normal hearing. If there is no echo, your baby might have hearing loss.

Figure 1. A Newborn undergoing a hearing screening.
2. The auditory brain stem response (ABR) or Brainstem Auditory Evoked Response (BAER) Test: It tests how the auditory nerve and brain stem (which carry sound from the ear to the brain) respond to sound. During this test, your baby wears a small earphones and has electrodes painlessly placed on his or her head. The electrodes adhere and come off like stickers and should not cause discomfort. Because this test does not rely on a person’s response behavior, the person being tested can be sound asleep during the test. ABR focuses only on the function of the inner ear, the acoustic (hearing) nerve, and part of the brain pathways that are associated with hearing. For this test, electrodes are places on the person’s head (similar to electrodes placed around the heart when and electrocardiogram (EKG) is done), and brain wave activity in response to sound is recorded.
Full Hearing Test
All children who do not pass a hearing screening should have a full hearing test. This test is also called an audiology evaluation . an audiologist, who is expert trained to test hearing, will do the full hearing test. In addition, the audiologist will also ask questions about birth history, ear infection and hearing loss in the family.
Some of the test the audiologist might use include: Otoacoustic Emissions (OAE); ABR or BAER test (stated above); and behavioral audiometry evaluation.
3. Behavioral Audiometry Evaluation: It will test how a person responds to sound overall. Infants and toddlers are observed for changes in their behavior such as sucking a pacifier, quieting, or searching for the sound. They are rewarded for the correct response by getting to watch an animated toy (this is called visual reinforcement audiometry). Sometimes older children are given a more play-like activity (this is called conditioned play audiometry). Behavioral Audiometry Evaluation tests the function of all parts of the ear. The person being tested must be awake and must response to sounds heard cooperative during this tests.
Anatomy
A hearing loss happen when any part of the ear or auditory (hearing) system is not working in the usual way – Outer Ear, Middle Ear, Inner Ear, Auditory (ear) Nerve, Auditory (hearing) System.
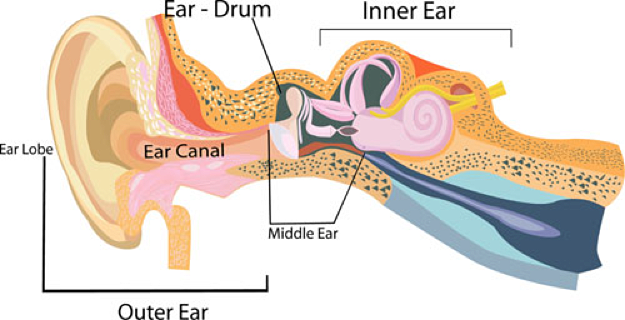
Figure 2. Ear and auditory (hearing) system.
Outer ear: It is made up of - the part we see on the sides of our heads, known as pinna, the ear canal, and the eardrum, sometimes called the tympanic membrane, which separates the outer and middle ear.
Middle ear: It is made up of - the eardrum and three small bones called ossicles that send the movement of the eardrum to the inner ear.
Inner ear: It is made up of - the snail shaped organ for hearing known as the cochlea, the semicircular canals that help with balance, and the nerves that go to the brain.
Auditory (ear) nerve: This nerve sends sound information from the ear to the brain.
Auditory (hearing) System: The auditory pathway processes sound information as it travels from the ear to the brain so that our brain pathways are part of our hearing.
Journey of Sound to the Brain
National Institute on Deafness and other Communication Disorders
https://www.nidcd.nih.gov/health/journey-of-sound-video
Types of Hearing Loss
There are four types of hearing loss:
- Conductive Hearing Loss: Hearing loss caused by something that stops sounds from getting through the outer or middle ear. This type of hearing loss can often be treated with medicine or surgery.
- Sensorineural Hearing loss: Hearing loss that occurs when there is a problem in the way the inner ear or hearing nerve works.
- Mixed Hearing Loss: Hearing loss that includes both a conductive and sensorineural hearing loss.
- Auditory Neuropathy Spectrum Disorder: Hearing loss that occurs when sound enters the ear normally, but because of damage to the inner ear or the hearing nerve, sound is not organized in a way that the brain can understand.
Degree of Hearing Loss
It can range from mild to profound.
- Mild Hearing Loss: A person with a mild hearing loss may hear some speech sounds but soft sounds are hard to hear.
- Moderate Hearing Loss: A person with a moderated hearing loss may hear almost no speech when another person is talking at a normal level.
- Severe Hearing Loss: A person with severe hearing loss will hear no speech when a person is talking at a normal level and only some loud sounds.
- Profound Hearing Loss: A person with a profound loss will not hear any speech and only very loud sounds.
Descriptions of Hearing Loss
Hearing loss can also be described as:
- Unilateral or Bilateral: Hearing loss is in one ear (unilateral) or both ears (bilateral).
- Pre-lingual or Post-lingual: Hearing loss happened before a person learned to talk (pre-lingual) or after a person learned to talk (post-lingual).
- Symmetrical or Asymmetrical: Hearing loss is the same in both ears (symmetrical) or is different in each ear (asymmetrical).
- Progressive or Stable: Hearing loss worsens over time (progressive) or happens quickly (sudden).
- Fluctuating or Stable: Hearing loss gets with better or worse over time (fluctuating) or stays the same over time (stable).
- Congenital or Acquired/Delayed Onset: Hearing loss is present at birth (congenital or appears sometime later in life (acquired or delayed onset).
Is Your Child "At Risk" for Hearing Loss?
If you checked one or more boxes below, your child may be at risk for hearing loss.
- Spent 5 days or more in the NICU or had complications while in the NICU. (Check with your health professionals).
- Needed special procedure (blood transfusion) to treat bad jaundice (hyperbilirubinemia).
- Was exposed to infection before birth.
- Has head, face or ears shaped or formed in a different way than usual.
- Has a condition (neurological disorder) that is associated with hearing loss (Check with your healthcare professional).
- Had an infection around the brain and spinal cord called meningitis.
- Received a bad injury to the head that required a hospital stay.
- Was given certain medications, like cancer chemotherapy or other medications that might hurt hearing. (Ask your healthcare professional).
- Your family has a history of children with hearing loss. Or
- You are worried about your child’s hearing for any reason.
Causes and Risk Factors
Hearing loss can happen anytime during life – from birth to adulthood. Following are some of the things that can increase the chance that a child will having hearing loss (1,2). 1 out of 4 cases of hearing loss in babies is due to maternal infections during pregnancy, complications after birth, and head trauma. For example, the child:
- Child was exposed to infection, such as, before birth;
- Spent 5 days or more in a hospital neonatal intensive care unit (NICU) or had complications while in NICU;
- Needed a special procedure like a blood transfusion to treat severe neonatal jaundice;
- Has head, face and ears shaped or formed in a different way than usual;
- Has a condition like a neurological disorder that may be associated with hearing loss;
- Had an infection around the brain (meningitis) and spinal cord;
- Received a bad injury to the head that required a hospital stay.
For about 1 out of 4 babies born with hearing loss, the cause is unknown.
Genetic Cause
About 1 out of 2 cases of hearing loss in babies is due to genetic causes. Some babies with a genetic cause for their hearing loss might have family members who also have a hearing loss. About 1 out of 3 babies with genetic hearing loss have a “syndrome.” This means they have other conditions in addition to hearing loss, such as Down syndrome or Usher syndrome. About 70% of all mutations causing hearing loss are non-syndromic. This means that the person does not have any other symptoms. About 30% of the mutations causing hearing loss are syndromic. This means that the person has other symptoms besides hearing loss. For example, some with hearing loss are also blind.
The cochlea (the part of the ear that changes sounds in the air into nerve signals to the brain) is a complex and specialized part of the body that needs many instructions to guide its development and function. These instructions come from genes. Changes in any one of these genes can result in hearing loss. The GJB2 gene is one the genes that contains the instructions for a protein called connexin 26; this protein plays an important role in the functioning of the cochlea. In some populations about 40% of newborns with a genetic hearing loss who do not have a syndrome, have a mutation of the GJB2 gene.
Details: https://www.cdc.gov/ncbddd/hearingloss/freematerials/parentsguide508.pdf
Cytomegalovirus & Hearing Loss
Some children with congenital cytomegalovirus (CMV) infection may have hearing or vision loss, or other health problems. CMV can be transmitted to an unborn baby during a woman’s pregnancy. Some babies with congenital CMV have hearing loss at birth in addition to other conditions. While some babies may have normal hearing initially, some will develop hearing loss later.
In this study delayed-onset and progression of sensorineural hearing loss (SNHL) in children with congenital CMV continued to occur throughout adolescence (3). However, the risk of developing SNHL after age 5 years among case-patients was not different than in uninfected children. Overall, 2% of case-patients developed SNHL that was severe enough for them to be candidates for cochlear implantation. In this study (3), from age 3 months to 5 years, the prevalence of SNHL doubled among case-patients from 7% to 14% but remained at 0% among controls.
The burden of CMV-related SNHL is substantial considering the potential impact of SNHL on children's development and academic achievement and their need for ongoing audiologic monitoring and interventions. There is estimate that 5% of children with asymptomatic congenital CMV infection, about 900 children annually, have SNHL >70 dB HL in at least 1 ear by age 12 months, and half of these children meet current candidacy criteria for cochlear implantation (4). As cochlear implant technologies and indications for their use continue to evolve, the number of children with asymptomatic congenital CMV infection and SNHL who might be considered candidates for cochlear implants could increase. Newborn screening for congenital CMV infection has potential to identify children at risk for CMV-related SNHL who currently go unrecognized and who might benefit from earlier intervention (5). Additional investigation into age of onset and risk factors for SNHL in children with asymptomatic congenital CMV infection are needed to inform the evaluation of the potential costs and benefits of CMV screening.
Auditory Neuropathy
Auditory neuropathy is a hearing disorder in which the inner ear successfully detects sound but has a problem with sending sound from the ear to the brain. It can affect people of all ages, from infancy through childhood. The number of people affected by auditory neuropathy is not known, but current information suggests that auditory neuropathies play a substantial role in hearing impairments and deafness (6).
When their hearing sensitivity is tested, people with auditory neuropathy may have normal hearing or hearing loss ranging from mild to severe. They always have poor speech-perception abilities, meaning that they have trouble understanding speech clearly. People with auditory neuropathy have greater impairment in speech perception than hearing health experts would predict based upon their degree of hearing loss on a hearing test. For example, a person with auditory neuropathy may be able to hear sounds but would still have difficulty recognizing spoken words. Sounds may fade in and out or seem out of sync for these individuals.
Risk factors of auditory neuropathy: There are several ways that children may acquire auditory neuropathy. Some children diagnosed with auditory neuropathy experienced particular health problems before or during birth or as newborns.
- Inadequate oxygen supply during or prior to birth, premature birth, jaundice, low birth weight, and dietary thiamine deficiency.
- Some drugs used to treat pregnant women or newborns may damage the baby’s inner hair cells, causing auditory neuropathy.
- Inheritance of mutated genes - Familial - scientists have identified genes with mutations that compromise the ear's ability to transmit sound information to the brain.
- Charcot-Marie-Tooth syndrome and Friedreich's ataxia. Neurological disorders that causes problems outside of the hearing system.
Meningitis and Hearing Loss
Bacterial meningitis is the most common cause for acquired hearing loss (7). Sensorineural hearing loss is a common sequela in children with bacterial meningitis. Identification of hearing loss in children with bacterial meningitis and early rehabilitation will lessen the long-term educational and social difficulties these children may experience (8). In this study, the overall incidence of sensorineural hearing loss in all patients with bacterial meningitis was 30.6% (8). A higher incidence of hearing loss was seen in children infected with S pneumoniae than N meningitis (35.9% and 23.9%, respectively) (9). This difference did not reach statistical significance. Preadmission antibiotics are associated with a decreased incidence of hearing loss in children with bacterial meningitis, decreased cerebrospinal fluid glucose, the presence of concurrent cranial nerve neuropathies, and length of hospitalization.
Congenital Unilateral Hearing Loss (UHL)
Congenital unilateral heating loss (UHL) has a prevalence ranging from 0.3 to 1.0 per 1,000 newborns (10). Before the advent of universal newborn hearing screening, UHL often went undiagnosed and unnoticed in children until they reached elementary school. The effect of UHL on speech and language development was as well as functionality and quality of life has been well-documented over the last 25 years. Research has shown that as many as 22% to 35% of children with UHL fail at least one school grade, and up to 20% are identified as having behavioral problems (11). Another study revealed that children with UHL experience barriers to their hearing that force them to adapt (10). In addition, quality-of-life studies have shown that children with UHL had a significantly larger variance in social functioning scores than children with normal bilateral hearing loss. Multiple studies have shown that the speech and language development delays can be ameliorated if appropriate intervention for children with hearing loss has begun (12).
In an attempt to diagnose and intervene earlier in children with hearing loss, the Joint Committee on Infant Hearing (JCIH) endorsed a "1-3-6 Plan," in which all infants will be screened no later than 1 month, have confirmation of hearing loss by 3 months, and receive intervention by 6 months (13). Despite these initiatives, nearly half of all infants who do not pass the initial hospital hearing screen do not receive timely, appropriate follow up care. A study found that the presence of co-occurring birth defects prolonged the time to initial hearing screening, resulting delays to diagnosis and intervention (14).
Risk factors for UHL (15):
- Craniofacial anomaly, was the most commonly reported (43.6%);
- Family history of permanent childhood hearing loss (21.8%);
- Stigmata associated with a syndrome including hearing loss was present in (18.2%);
- Neonatal indicators present in (12.7%) with UHL;
- In-utero infections present in 6.4%;
- Head trauma requiring hospitalization;
- Postnatal infections associated with SNHL and syndromes associated with progressive hearing loss;
- Cardiovascular system anomaly (12.4%) and ear-specific anomaly (7.0%).
The importance of congenital birth defects in this population is two-folds. First, the presence of a comorbid birth defect increases the chances that a child may need prolonged mechanical ventilator support. Multiple studies have demonstrated that mechanical ventilation greatly increases the likelihood of SNHL (16). The study also reported that application of mechanical ventilation can significantly damage the peripheral segment of the hearing tract. Second, the presence of a comorbid birth defect has been shown to lead to an increase in time to hearing screening, diagnosis, and intervention (17). In this study, a 3-year cohort study, 39,000 infants in the neonatal intensive care unit were 16.4 times more likely to miss the initial hearing screening and nearly 6 times more likely to miss their rescreen compared with infants in a well-baby nursery (18).
It is important to recognize children at risk for hearing loss and to perform screening and confirmatory testing in a timely manner despite the possible multitude of distracting congenital birth defects (19). The absence of risk factors does not preclude the development of UHL. Further studies are needed to define the etiology underlying UHL and better define the risk factor associations.
Early Hearing Screening Program for Infants and Children in U.S.
Prior to the establishment of a federal universal newborn infant hearing screening program in 1999, less than 10% of newborns in the U.S. were screened for hearing loss. As a result, 47% of children born with hearing loss were not diagnosed until their third birthday or later, missing a crucial period for language acquisition. In fact, children begin learning speech and language in the first six months of life, which is why early identification of hearing loss is critical (20). Research suggests that children with hearing loss who get help early develop better language skills than those who do not.

Figure 3. "1-3-6 Plan", to diagnose and intervene earlier in children with hearing loss.
In 2017 the Early Hearing Detection and Intervention (EHDI) law re-authorizes Health Resources and Service Administration (HRSA) to continue funding awards to states, territories, and healthcare providers to support continuous improvement of EHDI programs. These projects help to identify effective strategies to address screening, loss to follow-up diagnosis and services, enrollment into early intervention services, and family engagement. Project grants are also awarded to organizations to improve family-to-family support systems and to educate healthcare professionals who provide services to children who are deaf or hard-of-hearing (21).
On October 18, 2017, President Trump signed into law S. 652, EHDI Act (PL 115-71). The law amends the Public Health Service Act to re-authorize until 2022 a federal program administration by the U.S. Department of Health and Human Services (HHS). Three HHS agencies - the HRSA, the CDC, and the National Institutes of Health (NIH) - will continue a long-standing partnership to coordinate and advance a national program for the early identification and diagnosis of hearing loss and intervention services for deaf and hard-of-hearing newborns and infants. In addition, the law authorizes specific changes to the federal program, such as expanding the program to include young children who are at risk of losing their hearing during childhood from infection, harmful noise exposure, or genetic causes.
The law also encourages EHDI research programs at NIH through projects supported by the National Institute on Deafness and Other Communication Disorders (NIDCD). The NIDCD is committed to supporting biomedical research to improve both early hearing detection and intervention and hearing loss management, including screening, treatment, and rehabilitation (22). The law will allow for continued support of research on hearing aids, cochlear implants, speech perception and production, and language (both spoken and signed).
Collectively, HRSA, CDC, and NIH will enhance coordination so the federal EHDI program in U.S. and its territories, continues to ensure that infants who are deaf or hard-of-hearing are identified as early as possible and receive effective and timely interventions (23). These collaborations are critical to improving outcomes for affected children. HHS agencies will continue to promote essential services in order to minimize the negative impact that undiagnosed hearing loss can have on children’s speech, language, academic, social, and emotional development.
Aphasia
Aphasia is a disorder that results from damage to portions of the brain that are responsible for language. For most people, these areas are on the left side of the brain. It usually occurs suddenly, often following a stroke or head injury, but it may also develop slowly, as the result of a brain tumor or a progressive neurological disease. The disorder impairs the expression and understanding of language as well as reading and writing. Aphasia may co-occur with speech disorders, such as dysarthria or apraxia of speech, which also result from brain damage.
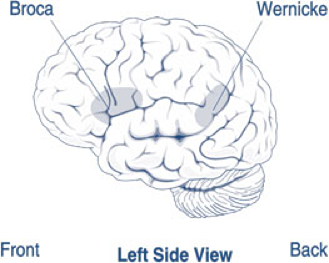
Figure 4. Areas of the brain affected by Broca’s and Wernicke’s aphasia.
About 1 million people in U.S. currently have aphasia, and nearly 180,000 Americans acquire it each year (24). There are two broad categories of aphasia: fluent and non-fluent, and there are several types within these groups. Damage to the temporal lobe of the brain may result in Wernicke's aphasia (shown in the picture above), the most common type of fluent aphasia. People with Wernicke's aphasia my speak in line, complete sentences that have no meaning, adding unnecessary words and even creating made-up words. Another hallmark of this type of aphasia is difficulty understanding speech.
The most common type of non-fluent aphasia is Broca's aphasia (see picture above). People with Broca’s aphasia have damage that primarily affects the frontal lobe of the brain. They often have right-sided weakness or paralysis of the arm and leg because the frontal lobe is also important for motor movements. People with Broca's aphasia my understand speech and know what they want to say, but they frequently speak in short phrases that are produced with great effort. They often omit small words, such as "is," "and" and "the."
Global aphasia, results from damage to extensive portions of the language areas of the brain. Individuals with global aphasia have severe communication difficulties and may be extremely limited in their ability to speak or comprehend language. They may be unable to say even a few words or may repeat the same words or phases over and over again. They may have trouble understanding even simple words and sentences.
There are other types of aphasia, each of which results from damage to different language areas in the brain. Conduction aphasia - these people have difficulty repeating words and sentences even though they understand them and can speak fluently. Anomic aphasia - people have difficulty naming objects even though they know what the object is and what it may be used for. Sometimes, blood flow to the brain is temporarily interrupted and quickly restored. When this type of injury occurs, which is called a transient ischemic attack, language abilities may return in a few hours or days.
Diagnosis: Most individuals will undergo a magnetic resonance imaging (MRI) or computed tomography (CT) scan to confirm the presence of a brain injury and to identify its precise location. If the physician suspects aphasia, the patient is usually referred to a speech-language pathologist, who performs a comprehensive examination of the person's communication abilities. The person's ability to speak, express ideas, converse socially, understand language, and read and write are all assessed in detail.
Aphasia therapy aims to improve a person's ability to communicate by helping him or her to use remaining language abilities, restore language abilities as much as possible, and learn other ways of communicating, such as gestures, pictures, and use of electronic devices. Individual therapy focuses on the specific needs of the person, while group therapy offers the opportunity to use new communication skills in a small-group setting.
Noise Induced Hearing Loss (NIHL)
NIHL can be caused by a one-time exposure to an intense "impulse" sound, such as an explosion, or by continuous exposure to loud sounds over an extended period of time, such as noise generated in a woodworking shop. Recreational activities that can put you at risk for NIHL include target shooting and hunting, snowmobile riding, listening to MP3 players at high volume through earbuds or headphones, playing in a band, and attending loud concerts. Sound is measured in units called decibels. Sounds at or below 70 A-weighted decibels (dBA), even after long exposure, are unlikely to cause hearing loss. However, long, or repeated exposure to sounds at or above 85 dBA can cause hearing loss. The louder the sound, the shorter the amount of time it takes for NIHL to happen.
Researchers have estimated that as many as 17% of teens (ages 12 to 19) have features of their hearing test suggestive of NIHL in one or both ears (25). Based on a 2011 - 2012 CDC study involving hearing tests and interviews with participants, at least 10 million adults (6%) in the U.S. under age 70 - and perhaps as many as 40 million adults (24%) - have features of their hearing test that suggest hearing loss in one or both ears from exposure to loud noise.
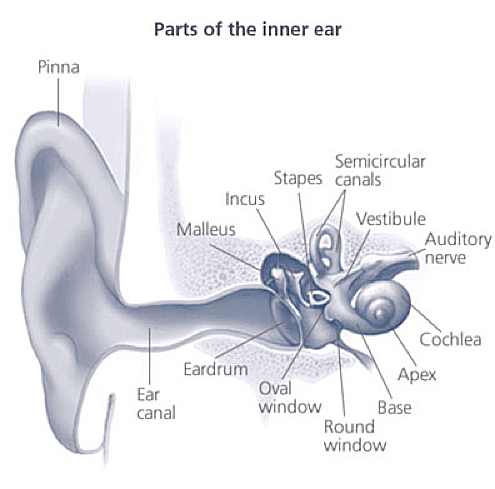
Figure 5. Parts of inner ear. Source: NIH Medical Arts
Once the vibrations cause the fluid inside the cochlea to ripple, a traveling wave forms along the basilar membrane. Hair cells - sensory cells sitting on top of basilar membrane ride the wave. As the hair cells move up and down, microscopic hair-like projections (known as stereocilia) that perch up on top of the hair cells bump against on overlying structure and bend. Bending causes pore-like channels, which are at the tips of the stereocilia, to open up. When that happens, chemicals rush into the cell, creating an electrical signal. The auditory nerve carries this electrical signal to the brain, which translates it into a sound that we recognize and understand.
NIHL is the only type of hearing loss that is completely preventable. If you understand the hazards of noise and how to practice good hearing health, you can protect your hearing for life. Protect the ears of children who are too young to protect their own. Known which noises can cause damage (those at or above 85 dBA. Noisy Planet is a national public education campaign designed to increase awareness among parents of children ages 8 to 12 about the causes and prevention of noise-induced hearing loss (26).
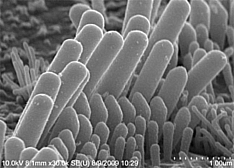
Figure 6. Stereocilia perch atop sensory hair cells in the inner ear.
Most NIHL is caused by the damage and eventual death these hair cells. Unlike bird and amphibian hair cells, human hair cells do not grow back. They are gone for good.
Loud noise exposure can also cause tinnitus - a ringing, buzzing, or roaring in the ears or head. Tinnitus may subside over time but can sometimes continue constantly or occasionally throughout a person’s life. Hearing loss and tinnitus can occur in one or both ears.
Prevention
Following are tips for parents to help prevent hearing loss in their children:
- Have a healthy pregnancy: prevent infections for baby's protection; get vaccinated - get the flu shot and the whooping cough vaccine. Become up-to-date with all vaccines before getting pregnant.
- Prevent insect bites: use insect repellent, wear long-sleeved shirts and long pants when outside and consider avoiding travel to areas with Zika and CMV virus infections.
- Practice good hygiene: wash your hands often with soap and water. Avoid putting a young child's cup or pacifier in your mouth.
- Make sure your child gets all the regular childhood vaccines. Available @ https://www.cdc.gov/vaccines/schedules/index.html
- Keep your child away from high noise levels, such as from very loud toys.
Types of Interventions
There are different types of communication options and interventions available for children with hearing loss. With help from healthcare providers and intervention specialists, families are able to select the options that best meet their needs. These are some of the possible options:
- Learning other ways to communicate, such as sign language.
- Technology to help with communication, such as hearing aids and cochlear implants.
- Medicine and surgery to correct some types of hearing loss.
- Family support services, such as support groups.
Early Intervention and Special Education
Early Intervention (0-3 years)
Hearing loss can affect child's ability to develop speech, language, and social skills. The earlier a child who is deaf or hard-of-hearing starts getting services, the more likely the child's speech, language, and social skills will reach full potential. Babies that are diagnosed with hearing loss should begin to get intervention services as soon as possible, but no later than 6 months of age. There are many services available through the individuals with Disability Education Improvement Act 2004 (IDEA 20004) (27). Services for children from birth through 36 months of age are called Early Intervention or Part C services. Even if your child has not been diagnosed with a hearing loss, he or she may be eligible for early intervention treatment services. The IDEA 2004 says that children under the age of 3 years (36 months) who are at risk of having developmental delays may be eligible for services. These services are provided through an early intervention system in your state. Through this system, you can ask for an evaluation.
Special Education (3 - 22 years)
Special education is instruction specifically designed to address the educational and related developmental needs of older children with disabilities, or those who are experiencing developmental delays. Services for these children are provided through the public-school system. These services are available through the individuals with Disabilities Education Improvement Act 2004 (IDEA 2004), Part B.
Early Hearing Detection and Intervention (EHDI) Program
Every state has an Early Hearing Detection and Intervention (EHDI) program. EHDI works to identify infants and children with hearing loss. EHDI also promotes timely follow-up testing and services or interventions for any family whose child has a hearing loss. If your child has a hearing loss or if you have any concerns about your child's hearing, call toll free 1-800-CDC-INFO or contact your local EHDI Program coordinator to find available services.
Technology
Technology does not "cure" hearing loss but may help a child with hearing loss to make the most of their residual hearing.
Hearing Aids: It makes sounds louder. They can be worn by people of any age, including infants. Babies with hearing loss may understand sounds better using hearing aids. This may give them the chance to learn speech skills at a young age.
There are many styles of hearing aids. They can help many types of hearing losses. A young child is usually fitted with behind-the-ear style hearing aids because they are better suited to growing ears. See the figure 7 below.
Bone-Anchored Hearing Aids: This type of hearing aid can be considered when a child has either a conductive, mixed, or unilateral hearing loss and is specifically suitable for children who cannot otherwise wear 'in the ear' hearing aids.

Figure 7. An infant with behind-the-ear style hearing aid.
Cochlear and Auditory Brainstem Implants: A cochlear implant is a small, complex electronic device that can help to provide a sense of sound to a person who is profoundly deaf or severely hard-of-hearing. The implant consists of an external portion that sits behind the ear and a second portion that is surgically placed under the skin (see figure 8 below).
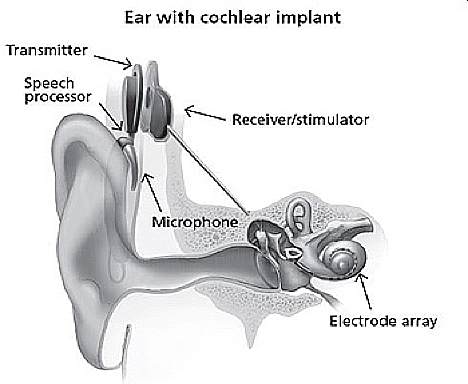
Figure 8. Ear with cochlear implant. Source: NIH/NIDCD.
An implant has the following parts:
- A microphone, which picks up sound from the environment.
- A speech processor, which selects and arranges sounds picked up by the microphone.
- A transmitter and receiver/stimulator, which receive signals from the speech processor and convert them into electric impulses.
- An electrode array, which is a group of electrodes that collects the impulses from the stimulator and sends them to different regions of auditory nerve.
An implant does not restore normal hearing. Instead, it can give a deaf person a useful representation of sounds in the environment and help him or her to understand speech.
The FDA first approved cochlear implants in mid-1980s to treat hearing loss in adults. Since 2000, cochlear implants have been FDA-approved for use in eligible children beginning at 12 months of age. For young children who are deaf or severely hard-of-hearing, using a cochlear implant while they are young exposes them to sounds during an optimal period to develop speech and language skills (28). Research has shown that when these children receive a cochlear implant followed by intensive therapy before they are 18 months old, they are better able to hear, comprehend sound and music, and speak than their peers who receive implants when they are older (28). Studies have shown eligible children who receive a cochlear implant before 18 months of age develop language skills at a rate comparable to children with normal hearing, and many succeed in mainstream classrooms (28).
Other Assistive Devices: Besides hearing aids, there are other devices that help people with hearing loss. Following are some examples of other assistive devices:
- FM system - It is a kind of device that helps people with hearing loss hear in background noise. FM stands for frequency modulation. It is the same type of signal used for radios. FM systems send sound from a microphone used by someone speaking to a person wearing the receiver. This system is sometimes used with hearing aids. An extra piece is attached to the hearing aid that works with the FM system.
- Captioning - Many television programs, videos, and DVDs are captioned. Television sets many after 1993 are made to show the captioning. You do not have to buy anything special. Captions show the conversation spoken in soundtrack of program on the bottom of the television screen.
- Other devices - there are many other devices available for children with hearing loss. Some of these include text messaging, telephone amplifiers, flashing and vibrating alarms, audio loop systems, infrared listening devices, portable sound amplifiers, TTY (Text Telephone or teletypewriter).
Medical and Surgical Management
One type of conductive hearing loss can be caused by a chronic ear infection. A chronic ear infection is a build-up of fluid behind the eardrum in the middle ear space. Most ear infections are managed with medication or careful monitoring. Infections that do not go away with medication can be treated with a simple surgery that involves putting a tiny tube into the eardrum to drain the fluid out.
Another type of conductive hearing loss is caused by either the outer or middle ear not forming correctly while the baby was growing in-utero. Both the outer and middle ear need to work together in order for sound to be sent correctly to the inner ear. This problem may be improved and perhaps even corrected with surgery. An otolaryngologist usually takes care of this problem placing a cochlear implant, auditory brainstem implant, or bone-anchored hearing aids will also require a surgery.
Learning Language and Communication Tools
Families who have children with hearing loss often need to change their communication habits or learn special skills (such as sign language) to help their children learn language. These skills can be used together with hearing aids, cochlear or auditory brainstem implants, and other devices that help children hear.
Following are language approaches, and the skills that are sometimes included in each of them:

Figure 9. A: American Sign Language (ASL); B: Finger Spelling.
- Auditory-Oral: Natural gestures, listening, speech (lip) reading, and spoken speech;
- Auditory-Verbal: Listening, spoken speech;
- Bilingual: American Sign Language and English;
- Cued Speech: Cueing, Speech (Lip) Reading;
- Total Communication: Conceptually Accurate Signed English (CASE), Signing Exact English (SEE), Finger Spelling, Listening, Manually Coded English (MCE), Natural Gestures, Speech (Lip) Reading, Spoken Speech.
American Sign Language (ASL)
American Sign Language (ASL) is a language itself (29). While English and Spanish are spoken languages, ASL is a visual language. It is a complete language. People communicate using hand shapes, direction and motion of the hands, body language, and facial expressions. ASL has its own grammar, word order, and sentence structure. People can share feelings, jokes, and complete ideas using ASL. A baby can learn ASL as a first language.
Manually Coded English (MCE)
Manually Coded English (MCE) is made up of sings that ear a visual code for spoken English. MCE is a code for a language – the English language. Many of signs (hand shapes and hand motions) in MCE are borrowed from ASL. But unlike ASL, the grammar, word order, and sentence structure of MCE are similar to the English language. Children and adults can use many other communication tools along with MCE.
Conceptually Accurate Signed English (CASE)
Conceptually Accurate Signed English (CASE) (sometimes called Pidgin Signed English [PSE]) has developed between people who use ASL, and people who use MCE, using signs based on ASL and MCE. This helps them understand each other better. CASE is flexible and can be changed depending on the people using it. Other communication tools can be used with CASE. Often, finger spelling is used in combination with CASE.
Cued Speech
Cued speech helps people who are deaf or hard-of-hearing better understand spoken language when watching a person's mouth, many speech sounds look the same on the face even though the sounds heard are not the same. When "cueing" English, the person communicating uses eight hand shapes and four places near the mouth to help the person looking tell the difference between speech sounds. Cued speech allows the person to make out sounds and words when they are using other building blocks, such as speech reading (lip reading) or auditory training (listening).
Finger Spelling
With Finger Spelling the person uses hands and fingers to spell out words. Hand shapes represent the letters in the alphabet. Finger Spelling is used with many other communication methods; it is almost never used by itself. It is most often used with ASL, CASE, MCE to spell out words that do not have a sign, such as the names of places or people.
Natural Gestures
"Natural Gestures" - or body language - are actions that people normally do to help others understand a message. Babies will begin to use this building block naturally if they can see what others are doing. This building block is not taught, it just comes naturally. It is always used with other building blocks.
Listening/Auditory Training
Most people who are deaf or hard-of-hearing have some hearing. This is called "residual hearing". Some people rely or learn how to maximize their residual hearing (auditory training). This building block is often used in combination with other building blocks (such as hearing aids, cochlear implants, and other assistive devices). Listening might seem easy to a person with hearing. But for a person with hearing loss, Listening is often hard without proper training. Like all other tools, the skill of Listening must be learned.
Spoken Speech
People can use speech to express themselves. Speech is a skill that many people take for granted. Learning to speak is a skill that can help build language. Speech or learning to speak is often used in combination with hearing aids, cochlear implants, and other assistive devices that help people maximize their residual hearing. A person with some residual hearing may find it easier to learn speech than a person with no residual hearing. Like all other communication tools, the skill of speaking must be learned.
Speech Reading
Speech Reading (or lip reading) helps a person with hearing loss understand speech. The person watches the movements of a speaker’s mouth and face and understands what the speaker is saying. About 40% of the sounds in the English language can be seen on the lips of a speaker in good conditions, such as a well-lit room where the child can see the speaker’s face. But some words cannot be read. A good speech reader might be able to see only 4 to 5 words in a 12-word sentence. Children often use speech reading in combination with other tools, such as auditory training (listening), cued speech, and others. But it cannot be successful alone. Babies will naturally begin using this building block if they can see the speaker’s mouth and face. But as a child gets older, he or she will still need some training.
Global Hearing Health Care
The global prevalence of sensorineural hearing impairment was first reported by the World Health Organization (WHO) in 1985. At that time, 42 million people (approximately 1% of the world’s population) were estimated to have moderate to profound (or disabling) hearing impairment. By 2011, the estimate rose to 360 million, of whom 32 million were children younger than 15 years. The most recent WHO estimate suggests that approximately 466 million (or 6.1% of the world’s population) were living with disabling hearing loss, in 2018. This estimate is projected to rise to 630 million by 2030 and to over 900 million by 2050 (30). The Global Burden of Disease study, which incorporated mild and unilateral hearing loss, estimated that the population with hearing loss rose from 1.2 billion (17.2%) in 2008 to 1.4 billion (18.7%) in 2017. This trend has become a serious public health issue that deserves an appropriate and well-coordinated global action (30). Hearing loss is the fifth leading cause for years lived with disability worldwide, mainly due to its impact on interpersonal communication, cognition, education, employment, and social participation. Moreover, un-addressed hearing loss poses a huge global financial burden, costing over 750 billion USD annually (31).
The 2017 World Health Assembly Resolution Prevention of deafness and hearing loss, calls on Member States across all regions for stronger action in this field. This resolution has led several Member States to strengthen their ear and hearing care services while others are starting to develop public health strategies on hearing loss. However, challenges including lack of trained workforce, inadequate financial resources and low awareness still need to be met. These challenges can be tackled through the integration of ear and hearing care into health systems as part of universal health coverage (UHC). In 2015, when the United Nations General Assembly adopted the sustainable development goals, WHO and its Member States committed to achieve UHC by 2030. This target highlights the importance of primary health care and health system strengthening as the core approaches for delivering comprehensive person-centered care without causing financial hardship (32). Integrating ear and hearing care within these public health approaches is the key to ensuring sustainable and equitable access to services for everyone.
In practice, this integration would require implementing these strategies. First, including cost-effective interventions for ear and hearing care into mainstream health services. Second, training community health workers to raise awareness for hearing loss prevention and identification at the community level. This step could mitigate the stigma associated with this condition and ensure that people are able to access care for hearing loss and the common ear diseases that often lead to it. Third, developing effective policies for preventive measures like noise reduction and rational drug use. Fourth, ensuring access to sign-language education and hearing devices.
Summary
Some babies are born with hearing problems. Other children are born with normal hearing and begin to have hearing problems as they grow older. It is important to know what to expect as your baby grows, because hearing problems can delay the development of voice, speech, and language skills. Early Hearing Detection and Intervention Program (EHDI) enable states, territories, families, and healthcare providers to develop complete and coordinated systems of care so that newborns, infants, and young children who are deaf or hard-of-hearing are identified and get the care they need when they need it. Early involvement can help these children meet age-appropriate language, social, and other developmental milestones. Each year, 4.1 million newborns are screened for congenital disorders in the U.S. Of these, 4,000 infants are diagnosed as having a condition. It is estimated another 1,000 infants that have conditions go undetected. This resource is intended to promote comprehensive care through medical homes for children born with hearing loss. Ensure every newborn hearing screening results are communicated to all parents and reported in a timely fashion according to the state law, regulations, and guidelines. Incorporate EHDI into an integrated, medical home approach to child health.
References
- Centers for Disease Control and Prevention (CDC). Hearing loss in children: 2017 Hearing loss screening summary. Available @ https://www.cdc.gov/ncbddd/hearingloss/2017-data/01-data-summary.html Last accessed 2 June 2020
- Centers for Disease Control and Prevention. CDC's Development Milestones - from 2 months to 5 years; available @ https://www.cdc.gov/ncbddd/actearly/pdf/checklists/Checklists-with-Tips_Reader_508.pdf Last accessed 3 June 2020
- Lanzieri TM, Chung W. Flores M, Blum P, et al. Hearing loss with asymptomatic congenital cytomegalovirus infection. Pediatrics 2017, e20162610; DOI: https://doi.org/10.1542/peds.2016-2610
- Goderis J, De Leenheer E, Smets K, et al. Hearing loss and congenital CMV infection; a systematic review. Pediatrics 2014;134(5):972-982
- Demmler GJ. Screening for congenital cytomegalovirus infection: a tapestry of controversies. J Pediatr 2005;146(2):162-164
- National Institute on Deafness and Other Communication Disorder (NIDCD). Available @ https://www.nidcd.nih.gov/ Last accessed 2 June 2020
- Chang CJ, Chang HW, Chang WN, et al. Seizures complicating infantile and childhood bacterial meningitis. Pediatr Neurol 2004;31(3):165-171
- Kutz JW, Simon LM, Chennupati SK, et al. Clinical predictors of hearing loss in children with bacterial meningitis. Arch Otolaryngol Head Neck Surg 2006;132(9):941-945
- van Dommelen P, Mohangoo AD, Verkerk PH, et al. Neonatal Hearing Screening Working Group. Risk indicators for hearing loss in infants treated in different neonatal intensive care units. Acta Paediatr 2010;99(3):344-349
- Chapman DA, Stampfel CC, Bodurtha JN, et al. Impact of co-occurring birth defects on the timing of newborn hearing screening and diagnosis. Am J Audiol 2011;20(2):132-139
- Lieu JEC. Speech-language and educational consequences of unilateral hearing loss in children. Arch Otolaryngol Head Neck Surg 2004;130(5):524-530
- Sininger YS, Martinez A, Eisenberg L, et al. Newborn hearing screening speeds diagnosis and access to intervention by 20 - 25 months. Am J Acad Audiol 2009;20(1):49-57
- American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007;120(4):898-921
- White KR. The current status of EHDI programs in the United States. Ment Retard Dev Disabil Res Rev 2003;9(2):79-88
- Bielecki I, Horbulewicz A, Wolan T. Risk factors associated with hearing loss in infants: an analysis of 5282 referred neonates. Int J Pediatr Otorhinolaryngol 2001;75(7):925-930
- Martinez-Cruz CF, Poblano A, Fernandez-Carrocera LA. Risk factors associated with sensorineural hearing loss in infants at neonatal intensive care unit: 15-year experience at the National Institute of Perinatology (Mexico City). Arch Med Res 2008;39(7):686-694
- Bitsko RH, Visser SN, Schieve A, Ross DS, et al. Unmet health care needs among CSHCN with neurological conditions. Pediatrics 2009;124(suppl 4) S343-S351
- Vohr BR, Moore PE, Tucker RJ. Impact of family health insurance and other environmental factors on universal hearing screening program effectiveness. J Perinatol 2002;22(5):380-385
- Yelverton JC, Dominguez LM, Chapman DA, et al. Risk factors associated with unilateral hearing loss. JAMA Otolaryngol Head Neck Surg 2013;139(1):59-63
- O'Hollearn AS, Beavers T, Rex J, Cunningham AK et al. Restructuring data reported from State Early Hearing Detection and Intervention (EHDI) Programs: A Pilot Study. J of Early Hearing Detection and Intervention 2018;3(1):57-66
- Chung W, Beauchaine K, Grimes A, et al. Reporting newborn audiologic results to State EHDI Programs. Ear & Hearing 2017;38(5):638-642
- Chung W, Beauchaine K, Hoffman J, et al. Early Hearing Loss Detection and Intervention-Pediatric Audiology Links to Services EHDI-PALS: Building a National Facility Database. Ear & Hearing 2017;38:e227-e231
- Williams TR, Alam S, Gaffney M. Progress in identifying infants with hearing loss. MMWR; 2015;64(13):351-356
- National Aphasia Association (NAA). Learn about aphasia, 2020. Available @ http://www.aphasia.org Last accessed on 20 June 2020
- Henderson E, Testa MA, Hartnick C. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. Pediatrics 2011;127(1):e39-e46
- National Institute on Deafness and Other Communication Disorders (NIDCD). It's A Noisy Planet; Protect Their Hearing, 2020. Available @ https://www.noisyplanet.nidcd.nih.gov/ Last accessed on 12 June 2020
- U.S. Department of Education. Individuals with Disabilities Education Act (IDEA). Building the Legacy: IDEA 2004. Available @ https://sites.ed.gov/idea/ Last accessed on 22 June 2020
- U.S. Food & Drug Administration. Cochlear Implants. 2018; Available @ https://www.fda.gov/medical-devices/implants-and-prosthetics/cochlear-implants Last accessed 2 June 2020
- Centers for Disease Control and Prevention (CDC). American Sign Language (ASL) 2019; Available @ https://www.cdc.gov/ncbddd/hearingloss/parentsguide/building/asl.html Last accessed 2 June 2020
- Davis AC, Hoffman HJ. Hearing loss: rising prevalence and impact. Bulletin of the World Health Organization 2019;97:646-646A
- Global costs of unaddressed hearing loss and cost-effectiveness of interventions. A WHO report. Geneva: World Health Organization; 2017. Available @ https://apps.who.int/iris/bitstream/handle/10665/254659/9789241512046-eng.pdf Last accessed 12 June 2020
- Chadha S, Kamenov K, Cieza A. Health system requirements for hearing services. Bull World Health Organ 2019;97:647-647A
Published: 5 September 2020
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


