慢性肾脏病和妊娠
WHEC实践公报和临床管理准则的医疗保健提供商。教育补助金所提供妇女保健和教育中心( WHEC ) 。
Chronic kidney disease represents a heterogenous group of disorders characterized by alterations in the structure and function of the kidney. Its manifestations are largely dependent on the underlying cause and severity of the disease, but typically include decreased function, hypertension, and proteinuria, which can be severe. Etiologies are many, but examples of renal disorders common in young women include glomerular diseases (i.e. immunoglobulin A nephropathy, minimal change disease, and focal segmental glomerulonephritis), vascular diseases (i.e. thrombotic microangiopathies), tubulointerstitial diseases (i.e. nephrolithiasis and reflux nephropathy), and cystic diseases (i.e. polycystic kidney disease). Further, systemic diseases including diabetes, vasculitis, and systemic lupus erythematous often involve the kidneys. Chronic kidney disease significantly increases the risk of adverse maternal and perinatal outcomes, and these risks increase with the severity of the underlying renal dysfunction, degree of proteinuria, as well as the frequent coexistence of hypertension. More frequent prenatal assessments by an expert multidisciplinary team are desirable for the care of this particularly vulnerable patient population. Obstetricians represent a critical component of this team responsible for managing each stage of pregnancy to optimize both maternal and neonatal outcomes, but collaboration with nephrology colleagues in combined clinics wherein both specialists can make joint management decisions is typically very helpful. Strategies for optimization of pregnancy outcomes include meticulous management of hypertension and proteinuria where possible and the initiation of preeclampsia prevention strategies, including aspirin.
The purpose of this document is to discuss current management of pregnant patients with chronic kidney diseases, early diagnosis and postpartum management. Renal transplantation and pregnancy is also discussed. Avoidance of nephrotoxic and teratogenic medications is necessary, and renal dosing of commonly used medications must also be considered. The effect of pregnancy on kidney disease may manifest as a loss of renal function, particularly in the context of concomitant hypertension and proteinuria, and chronic kidney disease, even when mild, contributes to the high-risk of adverse pregnancy outcomes, including increased risks of preeclampsia, preterm delivery, and small-for-gestational age neonates.
Incidence and Background
The global prevalence of chronic kidney disease has been recently estimated to be approximately 13.4%, with a higher prevalence in women compared with men (1). Although the prevalence of chronic kidney disease in women of childbearing age seems relatively low, with estimates on the order of 0.1 - 4%, the implications of pregnancy in the context of chronic kidney disease are many and severe (2).
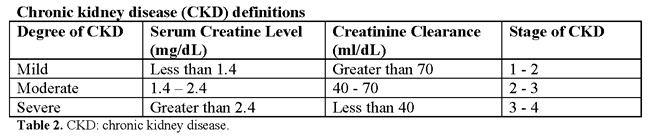
Chronic kidney disease is now widely classified into five stages according to the level of renal function.
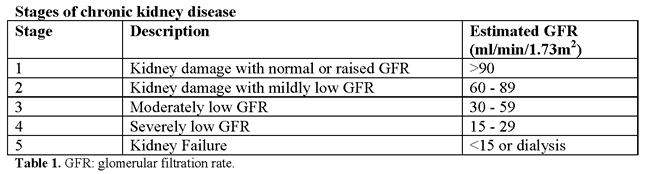
Stages 1 and 2 (normal or mild impairment with persistent albuminuria) affect up to 3% of women of child-bearing age (20-39 years). Stages 3-5 (glomerular filtration rate <60 ml/min) affect around 1 in 150 women of child-bearing age (3). Because of reduced fertility and an increased rate of early miscarriage, pregnancy in these women is less common. Studies of chronic kidney disease in pregnancy have mostly classified women on the basis of serum creatinine values, but the review of literature suggest that around 1 in 750 pregnancies is complicated by stages 3-5. Some women are found to have chronic kidney disease for the first-time during pregnancy. Around 20% of women who develop early preeclampsia (<30 weeks' gestation), especially those with heavy proteinuria, have previously unrecognized chronic kidney disease.
Renal Anatomic Changes with Pregnancy
Anatomic changes include dilatation of the renal collecting system (calices, renal pelvis, and ureters), which peaks by 20 weeks of gestation (4). These changes occur as a result of the effect of progesterone, which reduces ureteral tone, peristalsis and contraction pressure even early in pregnancy, as well as mechanical compressive forces that occur as the ureters cross the pelvic brim as pregnancy progresses. Hydronephrosis is seen predominantly on the right side, attributed to the crossing of the right ureter over the iliac and ovarian vessels at an angle before entering the pelvis. In contrast, the left ureter travels at a less acute angle in parallel with the ovarian vein. Kidney length increases by approximately 1 - 1.5 cm, and kidney volume increases up to 30% (4). Therefore, the diagnosis of true obstruction can be difficult, and in women at risk (e.g. obstructive or reflux nephropathy), surveillance ultrasound scans can be helpful. Further, this dilatation is responsible for the increased risk of pyelonephritis after asymptomatic bacteriuria, and regular screening for urinary tract infection is recommended in at-risk patients (e.g. advanced chronic kidney disease, chronic immunosuppression) (2).
Renal Physiologic Changes with Pregnancy
Owing to alterations in the hormones that govern vasodilation and vasoconstriction, several important hemodynamic changes also occur during pregnancy, most notably in systemic vascular resistance. This in turn leads to a decrease in mean arterial pressure, which typically begins in the first trimester with a nadir at 18-24 weeks of gestation, returning to baseline close to term. As such, women with mild hypertension may be able to discontinue medication in the early stages of pregnancy. In contrast, poorly controlled hypertension preconception and in early pregnancy portends a particularly poor prognosis (5).
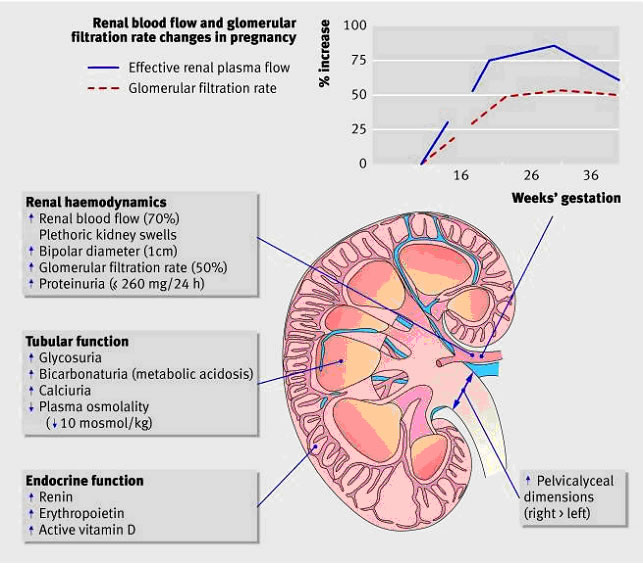
Figure 1: Physiological changes to the kidney during healthy pregnancy
Renal vasodilatation increases renal plasma flow, and hence the glomerular filtration rate (GFR). Glomerular hyperfiltration is the most significant physiologic change associated with normal pregnancy, presenting clinically as a decrease in the serum creatinine level. An estimation of GFR is important in the diagnosis and management of kidney dysfunction during pregnancy. The inverse hyperbolic relationship between serum creatinine and GFR is blunted at the higher range of the GFR, which typifies pregnancy. In a study that measured GFR by proper clearance methodology in women with preeclampsia and in healthy gravid controls, a comparison of the serum creatinine level with the GFR revealed a profound depression in kidney function in women with preeclampsia that could not be easily appreciated by evaluation of the serum creatinine level (6).
Modification in tubular function also occurs in normal pregnancies, with alterations seen in the tubular handling of glucose, amino acids, and uric acid. The most clinically relevant adaption is the alteration in protein excretion, wherein increased proteinuria is often attributed to hyperfiltration. Throughout pregnancy, the value for significant protein excretion is that which exceeds 300 mg in a 24-hour period (double the upper limit of normal in healthy adult). However, it should be highlighted that this upper limit has not been well-studied. One of the largest studies established 24-hour urinary excretion of total protein in 270 healthy pregnancies, reporting that mean 24-hour protein excretion was 116.9 mg with an upper 95th CI of 259.4 mg (6),(7). Because convincing evidence for significant glomerular leakage of protein in a normal pregnancy is insufficient, significant proteinuria should not necessarily be attributed to the hyperfiltration of pregnancy and requires assessment.
Effects of Pregnancy on Kidney Disease
One of the most important considerations in the management of pregnancy in the context of chronic kidney disease is the potential for pregnancy to hasten disease progression and decrease the time to end-stage renal disease. Women with chronic kidney disease are less able to make the renal adaptations needed for a healthy pregnancy. Their inability to boost renal hormones often leads to normochromic normocytic anemia, reduced expansion of plasma volume, and vitamin D deficiency (8).
Mild renal impairment (stages 1 - 2): Most women with chronic kidney disease who become pregnant have mild renal dysfunction and pregnancy does not usually affect renal prognosis. A case-control study of 360 women with primary glomerulonephritis and mild renal dysfunction (serum creatinine <110 μmol/l), minimal proteinuria (<1g/24h), and absent or well controlled hypertension before pregnancy showed that pregnancy has little or no adverse effect on long term (up to 25 years) renal function in the mother (9).
Moderate to severe renal impairment (stages 3 - 5): Small mainly uncontrolled retrospective studies have shown that women with the worst renal function before pregnancy are at greatest risk of an accelerated decline in renal function during pregnancy. Preexisting proteinuria and hypertension both increase this risk (10). A prospective study assessing the rate of decline of maternal renal function during pregnancy in 49 women with chronic kidney disease stages 3-5 before pregnancy confirmed a decline in renal function during the third trimester, which persisted in most women and deteriorated to end stage renal failure (11). Women with both an estimated GFR <40 ml/min/1.73 m2 and proteinuria >1g/24 h before pregnancy showed an accelerated decline in renal function during pregnancy. Chronic hypertension predisposes women to preeclampsia - this may explain why some women with milder renal function dysfunction also have a gestational decline in renal function. The risk of such a decline is reduced when hypertension is controlled.
Effects of Kidney Disease on Pregnancy
As important as it is to consider the effect of pregnancy on the course of maternal chronic kidney disease, it is of equal importance to contemplate the effect of chronic kidney disease on pregnancy outcomes, because the degree of renal function impairment in addition to the presence of hypertension and proteinuria are also major determinants of poor maternal and perinatal outcomes. In women with renal insufficiency, the presence of GFR less than 40 mL/min/1.73 m2 and proteinuria with protein greater than 1 g/d before conception predicts poor maternal and fetal outcomes (11),(12). Outcomes examined included risk of cesarean delivery, preterm delivery at less than 34 weeks of gestation, small for gestational age (SGA), and need for neonatal intensive care unit (NICU) admission. The risk of adverse outcomes increased across stages of chronic kidney disease, with a general combined outcome (preterm delivery, NICU and SGA) of 21% compared with 80% for stage 1 compared with stage 4-5 chronic kidney disease, respectively. In those with advanced chronic kidney disease, significantly higher rates of cesarean delivery, preterm delivery at less than 37 or less than 34 weeks of gestation, as well as SGA less than the 10th and less than the 5th percentile have been described (13). Women with more advanced chronic kidney disease also are more likely to have higher rates of concomitant hypertension and proteinuria, which further increases the risk of adverse pregnancy outcomes.
OPTIMIZATION STRATEGIES
Given the heightened risk for both adverse maternal and neonatal outcomes in women with chronic kidney disease, in particular those with advanced disease, multidisciplinary care that includes nephrologists, maternal-fetal medicine specialists, neonatologists, and a specialized NICU is the ideal. Despite the inherent risks, several management strategies exist to optimize outcomes, beginning with preconception care through delivery and then extending into the postpartum period. These principles of management are summarized below:
Hypertension Management
Currently no randomized controlled trials exist to establish optimal blood pressure targets among patients with chronic kidney disease in the context of pregnancy; however, extrapolation from the CHIPS (Control of Hypertension in Pregnancy Study) trial is likely reasonable. In this study randomized women were advised to target a diastolic blood pressure of 85 mm Hg (tight control) compared with 100 mm Hg (less tight control) and found no significant difference in risks of adverse pregnancy outcomes between the groups; however, those with less tight control were more likely to develop severe hypertension (greater than 160/110 mm Hg) (14). Blood pressure levels of this magnitude may lead to further kidney damage. Thus, a blood pressure target of less than 140/90 mm Hg has been recommended for women with chronic kidney disease during pregnancy.
- Safe options:
- Methyldopa (maximum 3 g in divided doses)
- Labetalol (maximum 1.2 g in divided doses)
- Nifedipine XL (maximum 90 mg twice/d)
- Hydralazine (50 mg every 6 h)
- Unsafe options:
- Angiotensin-converting enzyme inhibitors
- Angiotensin receptor blockers
- Goal less than 140/90 mm Hg
Proteinuria Management
Kidney biopsy is feasible in pregnancy but rarely necessary if the woman has received adequate preconception counseling, which includes a biopsy for definitive diagnosis. Biopsy is, therefore, typically done only in early gestation, and indications may include new-onset nephrotic syndrome, significant glomerular disease wherein confirmation of diagnosis will affect treatment choice, or a sudden deterioration in renal function. Beyond approximately 30 weeks of gestation, however, the risks of kidney biopsy may supersede its benefits owing to technical challenges associated with a gravid uterus and the potential for coexistent preeclampsia. Once a diagnosis is ascertained, options for management include several pregnancy-safe choices for diseases typically treated with immunosuppression (e.g. lupus nephritis, vasculitis, membranous nephropathy, minimal change disease) or, alternatively, renin-angiotensin-aldosterone system blockade discontinued before 8 weeks of gestation for diseases without immunologic treatment options (e.g. diabetic nephropathy, reflux nephropathy, hypertensive nephrosclerosis). As already mentioned, renin-angiotensin-aldosterone system blockade is teratogenic beyond 8 weeks of gestation (15).
- Biopsy preconception preferred, but if during pregnancy, before 32 weeks of gestation:
- For new-onset nephrotic syndrome or renal insufficiency
- If well-controlled blood pressure and no coagulopathy
- Safe immunosuppression:
- Prednisone
- Calcineurin inhibitors
- Azathioprine
- Unsafe immunosuppression:
- ? Rituximab - weigh risk-benefit
- Mycophenolate mofetil
- Cyclophosphamide
- Preconception renin-angiotensin-aldosterone system blockade
- Acceptable in select women with no immunologic treatment options
- Must stop at conception and no later than 8 weeks of gestation
- Nephrotic syndrome
- Edema
- Extremity elevation
- Furosemide (judicious use)
- Albumin infusions (severe cases)
- Anticoagulation with low-molecular-weight heparin
- Women with high-grade proteinuria with low serum albumin levels (less than 2.0 - 2.5 g/dL)
Pregnancy is a prothrombotic state, and in patients with severe hypoalbuminemia, there is a significantly increased risk of venous thromboembolic disease (16). No specific guidelines exist for the management of anticoagulation during pregnancy among those with chronic kidney disease and significant proteinuria, but expert opinion suggests that women with severe proteinuria and a serum albumin level of less than 2.0 - 2.5 g/dL should receive thromboprophylaxis throughout pregnancy and continued for at least 6 weeks postpartum (17). Anticoagulation also should be considered among those with lesser degrees of proteinuria with additional risk factors, including prolonged periods of immobility, obesity, or kidney diseases with higher risks of thrombosis (e.g. membranous nephropathy and vasculitis). The safety of sub-cutaneous low-molecular-weight heparin is well established for use in pregnancy.
Preeclampsia Prevention
The importance of preeclampsia cannot be understated, because with chronic kidney disease are among the highest risk patients for this serious complication. There have been no randomized controlled trials in preeclampsia prevention conducted specifically in the chronic kidney disease population, but options, including aspirin and calcium supplementation are generally safe. Because the population with chronic kidney disease is at high risk for the development of preeclampsia, aspirin should be initiated before 16 weeks of gestation, and with findings from the recent ASPRE (Combined Multimarker Screening and Randomized Patient Treatment with Aspirin for Evidence-Based Preeclampsia Prevention) trial, there is the suggestion that perhaps a higher dose (e.g. 150 mg) may be more effective (18).
- Low-dose acetylsalicylic acid
- 100 - 150 mg
- Before 16 weeks of gestation
- Stop at 34 - 36 weeks of gestation
- Calcium supplementation
- 1.5 - 2 g total
Calcium and vitamin D supplementation also have been evaluated as preventive strategies for preeclampsia. A systematic review included randomized controlled trials comparing high-dose (at least 1 g daily of calcium) or low-dose calcium supplementation during pregnancy with placebo or no calcium in the prevention of preeclampsia (19). The assessment of high-dose calcium greater than 1 g/d included 13 studies and 15,370 women, noting that the risk of hypertension was reduced with calcium supplementation compared with placebo, along with significant reduction in the risk of preeclampsia.
More recently, the benefit of vitamin D and calcium supplementation in pregnancy of risk reduction of preeclampsia and gestational hypertension was assessed by a meta-analysis of 27 randomized controlled trials including approximately 28,000 women noting that calcium, vitamin D, and calcium plus vitamin D could lower the risk of preeclampsia when compared with placebo (20). The World Health Organization (WHO) recommends daily supplementation with 1.5 - 2 g of oral elemental calcium in populations with low dietary intake for prevention of preeclampsia, but vitamin D supplementation requires further study.
Other Neurological and Obstetrical Management
Other general management strategies in chronic kidney disease include avoidance of nephrotoxic agents and renal dosing for commonly used medications as well as management of anemia, bone mineral metabolism, and acid-base and electrolyte imbalances. Several commonly used medications for obstetric indications may be potentially nephrotoxic, and thus should be avoided. This includes tocolytic agents such as indomethacin in addition to commonly used antimicrobial agents such as gentamicin. The common use of nonsteroidal anti-inflammatory medications for postpartum pain control also should be avoided in women with renal dysfunction. Medications that undergo renal clearance (e.g. antimicrobial agents) typically require dose adjustments for a GFR less than 30 mL/min.
Magnesium, a frequently used medication for eclampsia prevention or fetal neuroprotection, is cleared by the kidneys, and as such, magnesium toxicity presents a significant risk in women with advanced chronic kidney disease, especially those on dialysis. Thus, regular assessment of serum magnesium concentrations and deep tendon reflexes and a lower constant infusion rate (e.g. 1 g/h) are often indicated.
Maternal anemia is common in women with chronic kidney disease, and early institution of oral iron, intravenous iron sucrose, or both in addition to erythropoietin-stimulating agents when pregnancy is recommended. Hypocalcemia and hyperphosphatemia due to secondary hyperparathyroidism from advanced chronic kidney disease can be treated safely with oral calcium carbonate supplementation, binders, or both as well as vitamin D analogues. Maternal acidosis will result in progressive fetal acidemia, and as such, maternal serum pH ideally should be maintained at greater than 7.2. This may require initiation of sodium bicarbonate therapy, and in extreme cases, is an indication for dialysis. Women with chronic kidney disease also may have electrolyte abnormalities, and dietary counseling for a low-potassium diet should be initiated first, but binding resins can be used if needed. Again, this may be an indication to initiate dialysis.
- Avoid nephrotoxins
- Nonsteroidal anti-inflammatory drugs
- Dose reduce renally cleared medications
- Cautious use of magnesium sulfate
- Fetal surveillance
- Serial biophysical profile, nonstress test or amniotic fluid index, or contraction stress test
- Serial growth assessment
Owing to increased risk of adverse pregnancy outcomes, more frequent prenatal assessments to allow for close maternal and fetal monitoring may be necessary. A significantly rapid and severe decline in renal function is an indication for preterm delivery or termination of pregnancy. Antepartum fetal surveillance should be conducted according to the guidelines (21). Review Antepartum Fetal Surveillance http://www.womenshealthsection.com/content/obs/obs005.php3
In the absence of maternal or fetal compromise, consideration should be given to delivery at or near term, with cesarean delivery for usual obstetric indications.
END-STAGE RENAL DISEASE (ESRD)
In the population of women with end-stage renal disease (ESRD) on dialysis, conception and maintenance of pregnancy were historically infrequent and complex events. Fertility rates are typically low in those on hemodialysis and even lower in women on peritoneal dialysis, thought to be due impaired pituitary release of luteinizing hormone contributing to anovulation (22). To date, the highest documented pregnancy incidence is 15.6% in eligible intensively dialyzed home dialysis patients who conceived between 2001 and 2006, and outcomes also have improved, with live birth rates exceeding 80% in centers using intensified dialysis regimens (23). There is positive relationship between number of hours on dialysis and improved outcomes, with a decreased risk of preterm delivery before 37 weeks of gestation and small-for-gestational-age neonates less than the 10th percentile (24). In those with ESRD and no residual renal function, current recommendations a minimum of 36 h/week, but in women with residual renal function, this intensified therapy may not be required, and the dialysis prescription should be personalized to meet specific needs.
Compared with normal women, pregnancies in uremic patients undergoing maintenance hemodialysis have a higher risk of adverse outcomes in mother and fetus, such as, spontaneous abortion, hypertension, preeclampsia, polyhydramnios, preterm labor, and premature birth (25). Since the first case of pregnancy and successful delivery of patients on hemodialysis in 1970s, with the continuous development and improvement of dialysis technologies and experiences, more and more successful cases have been reported. During the past years before pregnancy, the dialysis scheme of the uremic patients is usually 4-hour dialysis sessions 3 times weekly. During pregnancy intensive dialysis and multidisciplinary cooperation according to the recommendations in the available literatures on pregnant women is summarized below.
Firstly, the total weekly hemodialysis is increased from 12 to 20 hours weekly, the dialyzer with high efficiency biocompatible membrane is used, the average blood flow is maintained from 180 to 240 mL/min and the dialysate flow at 500 mL/min. Low-molecular weight-heparin (bolus dose of 1000 IU followed by 250 IU every hour) is used to minimize the hemorrhagic risk and avoid coagulation of the dialyzer (26).
Secondly, control of dry weight by slow continuous ultrafiltration in order to achieve the goal of 0.5 kg on weight gain per week is maintained.
Thirdly, in order to target the postdialysis blood pressure below 140/90 mm Hg and to avoid intradialytic hypotension (<120/70 mm Hg), the dialyzed pregnant women are treated by combination of ultrafiltration assessments and antihypertensive drugs, including long-acting calcium antagonist and alpha-methyldopa.
Fourthly, management of anemia. The patients are recommended to receive subcutaneous recombinant human erythropoietin at a dose of 10,000 IU twice per week and intravenous iron administration of iron-sucrose at a dose of 100 mg biweekly, as well as 10 mg of folic acid supplementation. In addition, nutritional support is also recommended for the pregnant women as follows: protein intake of 1 g/kg/d and 20 g/d more, calorie intake of 35 to 40 kcal/d. The dose of intake for calcitriol and calcium carbonate D3 is 0.25 μg/d and 0.6 g/d, respectively. With regard to the obstetric care, after the pregnancy is confirmed by pelvic ultrasound, the fetal biometries are assessed according to the guidelines. The single umbilical artery, polyhydramnios and fetal growth restriction and ultrasound for fetal anomalies needs to be followed.
Clearance of urea plays a crucial role in pregnancy success, and there exists correlation between blood urea levels and gestational age, with urea levels lower than 48 mg/dL being associated with a gestational age of at-least 32 weeks (27). In the absence of evidence of maternal or fetal compromise, induction of labor is considered at term (37-39 weeks of gestation) to avoid spontaneous labor in an anticoagulated woman. Delivery should take place in a center with resource necessary to care for complex maternal and fetal situations. Initiation of magnesium sulfate for prevention of preeclampsia or fetal neuroprotection in cases of preterm delivery must be prescribed with vigilance. Postpartum, breastfeeding is safe in women undergoing dialysis. Most medications that are compatible with pregnancy are also safe while breastfeeding, but providers also should be attentive to avoid over-aggressive ultrafiltration and dehydration, which might impede breast milk supply.
RENAL TRANSPLANTATION
Estimates indicate that the proportion of women with renal transplants who become pregnant is approximately 2% - 5% (28). Pregnancy rates are significantly lower than in the age-matched general population, and it is not clear whether this represents decreased fertility or counseling practices and patient choice (29). At this time, much of the information available to guide practice comes from single-center experiences and systematic reviews and through transplant registries. The recently published Transplantation Pregnancy Registry International 2015 Annual Report includes 1,892 pregnancies in kidney recipients and 109 in kidney-pancreas recipients and is the largest of the available registries providing data on both maternal and fetal outcomes (30). After kidney transplantation as in all chronic kidney disease stages, the degree of kidney impairment, hypertension and proteinuria are acknowledged factors in the pathogenesis of adverse pregnancy-related outcomes, even though their pathogenesis in incompletely understood.
The clinical choices in cases at high risk of malformations or kidney function impairment (pregnancies under mycophenolic acid or with severe kidney-function impairment) require merging clinical and ethical approaches in which, beside the mother and child dyad, the grafted kidney is crucial "third element." Bioethical aspects (31):
- Pregnancy is not a "zero-risk" choice. Grading the risks of pregnancy after kidney transplantation is difficult, in particular in cases that differ from the "ideal" candidate (strong suggestion, evidence from different sources, mainly epidemiological studies).
- Pregnancy after kidney transplantation poses important ethical problems (strong suggestion, beyond evidence).
- Pregnancy in "non-ideal" candidates after kidney transplantation is an example of bioethical conflict, in which the principles of ethical assessment may give rise to contrasting evaluation (strong suggestion, beyond evidence).
Which patients are the "best candidates" for pregnancy after kidney transplantation and which patients are not:
- The following are the requirements most often cited for identifying the best candidates for pregnancy after kidney transplantation from the clinical point of view:
- Normal or good kidney function (differently defined: usually as GFR above 60 ml/min)
- No proteinuria or scarce proteinuria (differently defined: usually as below 300-500 mg/day)
- No hypertension or well-controlled hypertension (the latter usually defined as treated in monotherapy and without organ damage)
- Low-dose immunosuppression with "allowed" drugs
- At least 2 years after kidney transplantation (this interval has recently been reduced to 1 year after kidney transplantation) (strong suggestion, several sources of observational data)
- Further clinical maternal elements that can contribute to identifying the "best candidates" include:
- No recent rejection episode
- No recurrent urinary tract infection
- Discontinuation of potentially teratogen drugs for at least 6 weeks (moderate suggestion, several sources of observational data and indirect evidence)
- From the obstetric point of view, besides the absence of hypertension, and kidney disease, a low-risk mother is young (under 35), non-obese, non-diabetic, with a spontaneous singleton pregnancy (strong suggestion, several sources of observational data and indirect evidence)
- All other cases are high-risk kidney transplantation pregnancies. No graduation of risks is presently available (strong suggestion, several sources of observational data and indirect evidence)
The Study Group therefore proposes an individualized evaluation in all the cases. A pregnant grafted woman has been defined as a complex chimera with at least three cell populations: her own one, the donor organ and the fetus. Previous pregnancies and blood transfusions may have added other cell populations. The tolerance system is complex and not all antigens induce a response; tolerance may be the result of exposure of particular antigens or complexes (32).
Pregnancy outcomes after renal transplantation are generally thought to be superior to those in women undergoing dialysis. Pregnancy complications occurs more commonly in renal transplant recipients as compared with the general population, including hypertension (54% vs 5%), preeclampsia (27% vs 3.8%), and gestational diabetes (8% vs 3.9%). Additional adverse outcomes include low birth weight, increased risk of cesarean delivery, and admission to NICU (33). Pregnancy in the third post-transplant year was not associated with an increased risk of graft loss. On the other hand, live birth rates tend to be higher in the first 2 years post-transplantation. A meta-analysis of outcomes of 4,700 pregnancies in renal transplant recipients indicated a higher live birth rate (80%) with a mean interval transplant and pregnancy of less than 2 years compared with intervals of 2-3 years, 3-4 years and more than 4 years (live birth rates 64%, 76%, and 75%, respectively) (34). However, for those conceiving less than 2 years post-transplant, higher risks of other adverse pregnancy outcomes, including preeclampsia, gestational diabetes, cesarean delivery, and preterm birth are reported. The American Society of Transplantation Guidelines provides some direction and recommends avoidance of conception in the first year of transplantation (35). Pregnancy is deemed safe if there has been no rejection within the past year, adequate and stable graft function as evidenced by serum creatinine levels less than 1.5 mg/dL, no or minimal proteinuria, no acute infections that may affect fetal growth and well-being, and stable maintenance immunosuppression with pregnancy safe medications.
Cesarean Delivery: In patients undergoing cesarean delivery, the obstetrician must be attentive to the location of the transplanted kidney and ureter by reviewing operative summaries as well as ultrasonographic imaging before delivery. Often the ureter is reimplanted at the dome of bladder, and thus a common recommendation is to avoid creation and development of a bladder flap at the time of cesarean delivery.
POSTPARTUM CARE
It can take up to 3 months, occasionally longer, for the physiological changes of pregnancy to disappear. During that time, close monitoring of fluid balance, renal function, blood pressure, and a further review of drug treatment are necessary. Women who have new onset proteinuria associated with preeclampsia should be followed until proteinuria disappears, or until a diagnosis of renal disease is made.
Breastfeeding should be encouraged in women with chronic kidney disease. Information is confusing as to the extent to which some immunosuppressive drugs - such as ciclosporin and tacrolimus - appear in breast milk (36). But prednisolone, azathioprine, and angiotensin converting enzyme inhibitors are barely detectable in breast milk. It is still unclear whether the benefits of breastfeeding are countered by neonatal absorption of immunosuppressive drugs. Most experts encourage mothers who want to breastfeed but are taking immunosuppressive drugs to do so as long as the baby is thriving.
Summary
Chronic kidney disease with pregnancy represents a unique and complex situation with increased risks of adverse maternal and perinatal outcomes. Women with mild renal dysfunction (stages 1 - 2) usually have an uneventful pregnancy and good renal outcome. Clinical features, in particular uncontrolled hypertension, heavy proteinuria (>1 g/24h), and recurrent urinary tract infections have an independent and cumulative negative effect on pregnancy. Women with moderate to severe disease (stages 3 - 5) are at highest risk of complications during pregnancy and of an accelerated decline in renal function. Successful management of women with chronic kidney disease during pregnancy requires teamwork between primary care clinicians, midwives, specialists, and the patient. Frequent monitoring of simple clinical and biochemical features will guide timely expert intervention to achieve optimal pregnancy outcome and conservation of maternal renal function.
Pregnancy is an added value for women with kidney transplantation; fertility is at least partly restored, and a successful pregnancy is possible, frequent, and usually successful. However, kidney transplantation pregnancies have a higher risk of thromboembolism, preterm delivery and small for gestational age babies than pregnancies in the general population. The side effect of this positive outlook is that evidence is heterogenous and sometimes difficult to interpret. This lack of certitudes should be borne in mind at counseling, and strongly supports shared choices in the context of multidisciplinary care, as well as individualized approaches.
References
- Hill NR, Fatoba ST, Oke JI, et al. Global prevalence of chronic kidney disease: a systematic review and meta-analysis. PLoS One 2016;11:e0158765
- Piccoli GB, Attini R, Cabiddu G, et al. Kidney diseases and pregnancy: a multidisciplinary approach for improving care by involving nephrology, obstetrics, neonatology, urology, diabetology, bioethics and internal medicine. J Clin Med 2018;7:E135
- Williams D, Davison J. Chronic kidney disease in pregnancy. BMJ 2008;336(7637):211-215
- Piccoli GB, Alrukhaimi M, Liu ZH, et al. World Kidney Day Steering Committee. What we do and do not know about women and kidney diseases; questions unanswered and answers unquestioned: reflection on World Kidney Day and International Woman's Day. Physiol Int 2018;105:1-18
- Nobles CJ, Mendola P, Mumford SL et al. Preconception blood pressure levels and reproductive outcomes in a prospective cohort of women attempting pregnancy. Hypertension 2018;71:904-910
- Koetje PM, Spaan JJ, Kooman JP, et al. Pregnancy reduces the accuracy of the estimated glomerular filtration rate based on Cockroft-Gault and MDRD formulas. Reprod Sci 2011;18:456-462
- Hladunewich MA, Myers BD, Derby GC, et al. Course of preeclamptic glomerular injury after delivery. Am J Physiol Ren Physiol 2008;294:F614-620
- Willams D. Renal disorders. In: James DK, Steer PJ, Weiner CP, Gonik B, eds. High risk pregnancy. Management options. 3rd ed. Philadelphia: Elsevier Saunders, 2006;1098-1124
- Fischer MJ. Chronic kidney disease and pregnancy: maternal and fetal outcomes. Adv Chronic Kidney Dis 2007;14(2):132-145
- Piccoli GB, Cabiddu G, Attini R, et al. Risk of adverse pregnancy outcomes in women with CKD. J Am Soc Nephrol 2015;26:2011-2022
- Imbasciati E, Gregorini G, Cabiddu G, et al. Pregnancy in CKD stages 3 to 5: fetal and maternal outcomes. Am J Kidney Dis 2007;49:753-762
- Bramham K, Parnell B, Nelson-Piercy C, et al Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ 2014;348:g2301
- Piccoli GB, Fassio F, Attini R, et al. Pregnancy in CKD: whom should we follow and why? Nephrol Dial Transpl 2012;27(suppl 3):iii111-118
- Magee LA, von Dadelszen P, Rey E, et al. Less tight versus tight control of hypertension in pregnancy. N Engl J Med 2015;372:407-417
- Bullo M, Tschumi S, Bucher BS, et al. Pregnancy outcome following to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension 2012;60:444-450
- Liu S, Rouleau J, Joseph KS, et al. Epidemiology of pregnancy-associated venous thromboembolism: a population-based study in Canada. J Obstet Gynecol Can 2009;31:611-620
- Barbour SJ, Greenwald A, Djurdjv O, et al. Disease-specific risk of venous thromboembolic events is increased in idiopathic glomerulonephritis. Kidney Int 2012;81:190-195
- Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med 2017;377:613-622
- Hofmeyr GJ, Duley L, Atallah A. Dietary calcium supplementation for prevention of preeclampsia and related problems: a systematic review and commentary. BJOG 2007;114:933-943
- Khaing W, Vallibhakara SA, Tantrakul V, et al. Calcium and vitamin D supplementation for prevention of preeclampsia: a systematic review and network meta-analysis. Nutrients 2017;9:E1141
- Antepartum fetal surveillance. Practice Bulletin No. 145. American College of Obstetricians and Gynecologists. Obstet Gynecol 2014;124:182-192
- Shahir AK, Briggs N, Katsoulis J, et al. An observational outcomes study from 1966 to 2008, examining pregnancy and neonatal outcomes from dialyzed women during data from the ANZDATA registry. Nephrology 2013;18:276-284
- Hlandunewich MA, Hou S, Odutayo A, et al. Intensive hemodialysis associates with improved pregnancy outcomes: a Canadian and United States cohort comparison. J Am Soc Nephrol 2014;25:1103-1109
- Piccoli GB, Minelli F, Versino E, et al. Pregnancy in dialysis patients in the new millennium: a systematic review and meta-regression analysis correlating dialysis schedules and pregnancy outcomes. Nephrol Dial Transpl 2015;31:1905-1934
- Kendrick J, Sharma D, Holmen J, et al. Kidney disease and maternal and fetal outcomes in pregnancy. Am J Kidney Dis 2015;66:55-59
- Cao Y, Zhang Y, Wang X, et al. Successful pregnancy and delivery in uremic patients with maintenance hemodialysis. Medicine 2018;97(50):e13614
- Asamiya Y, Otsubo S, Matsuda Y, et al. The importance of low blood urea nitrogen levels in pregnant patients undergoing hemodialysis to optimize birth weight and gestational age. Kidney Int 2009;75:1217-1222
- McKay DB, Josephson MA. Pregnancy in recipients of solid organs - effects on mother and child. N Engl J Med 2006;354:1280-1293
- Hui D, Hladunewich MA. Chronic kidney disease and pregnancy. Obstet Gynecol 2019;133:1182-1194
- Coscia LA, Constantinescu S, Carlin FR, et al. 2015 Annual Report for the National Transplantation Pregnancy Registry (issued June 15, 2016). Available at http://www.transplantpregnancyregistry.com Retrieved 26 June 2019
- Cabiddu G, Spotti D, Gernomne G, et al. A best-practice position statement on pregnancy after kidney transplantation: focusing on the unsolved questions. The Kidney and Pregnancy Study Group of the Italian Society of Nephrology. J Nephrol 2018;31(5):665-681
- Ma KK, Petroff MG, Coscia LA, et al. Complex chimerism: pregnancy after solid organ transplantation. Chimerism 2013;4(3):71-77
- Rao D, Ghanta M, Moritz MJ, Constantinescu S. Long-term functional recovery, quality of life, and pregnancy after solid organ transplantation. Med Clin North America 2016;100:613-629
- Deshpande NA, James NT, Kucirka LM, et al. Pregnancy outcomes in kidney transplant recipients: a systematic review and meta-analysis. Am J Transpl 2011;11:2388-2404
- McKay DB, Josephson MA, Armenti VT, et al. Reproduction and transplantation: report on the AST Consensus Conference on reproductive issues and transplantation. Am J Transpl 2005;5:1592-1599
- Colla L, Diena D, Rossetti M, et al. Immunosuppression in pregnant women with renal disease: review of the latest evidence in the biologics era. J Nephrol 2018;31(3):361-383
发布时间: 16 October 2019
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


