Renal Disorders and Pregnancy
Dr. Jonathan Slater, MD, FACP
Pioneer Valley Nephrology
Springfield, MA (USA)
Among the various physiologic alterations that occur in normal pregnancy, few are as striking as those affecting the urinary tract. Changes in the urinary tract during normal pregnancy are so marked that norms in the nonpregnant cannot be used for obstetric management. Awareness of all alterations is essential if kidney problems in pregnancy are to be suspected or detected and then handled correctly. Most women with mild to moderate renal disease tolerate pregnancy well and have a successful obstetric outcome without adverse effect on the natural history of the underlying renal lesion. Crucial determinants are renal functional status at conception, the presence or absence of hypertension, and the type of renal disease.
These changes and various pitfalls for the unwary clinician are discussed in this chapter. There is no doubt that improvements in our knowledge of background physiology, in prenatal care generally, in technology for fetal surveillance, and in neonatal intensive care have meant better care for women with renal problems and their newborns.
- Normal Kidney Function:
- Blood Cleaning
- Protein in the Urine
- Hypertension (HTN) in Pregnancy
- Infection of the Urinary Tract
- Renal Failure
- The Basics
- Acute Renal Failure (ARF)
- Chronic Renal Failure (CRF)
- Pregnancy in CRF
Normal Kidney Function:
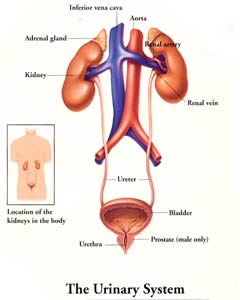
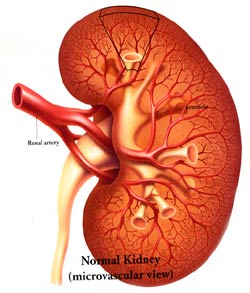
The main function of kidney is, to continuously clean the blood all the time. The blood is pumped from the heart (about 20% of all the blood is pumped out of the heart goes to the kidneys) and goes to the kidneys via the arteries known as renal arteries. The kidneys separate out the impurities (wastes that are continuously building up in the body as consequences of body metabolism) and also the water/fluids that accumulate are also separated out by the kidney to prevent body swelling and together this is the urine. THE URINE IS MADE IN THE KIDNEYS.
The urine is then delivered to the bladder via straw like structures called the ureters. The bladder is like a muscle sac that stretches to accommodate the urine and then when we urinate, the bladder contracts and the urine is expelled out via another small tube called the urethra that connects the bladder to the outside world.
The kidney is a very complicated organ that adjusts its function depending on the body's situation. For example: if you drink a lot of fluids the kidney makes a lot of urine to prevent swelling (e.g. drinking lot of beer). On the other hand if one does not drink much fluid, then the urine becomes very concentrated.
During pregnancy the kidneys also adapt to their new state and actually increase the functioning by cleaning the blood more than usual. This is detected by examining blood levels of markers we use to roughly evaluate how "clean" the blood is. We use the blood creatinine (Cr) and blood urea nitrogen levels (BUN) to do this. To get a more precise evaluation of the kidney's cleaning of the blood we can measure in the 24 hour urine collection for creatinine and protein. Serum levels of creatinine (Cr) and blood urea nitrogen (BUN), which average 0.8 mg/100 ml and 13 mg/100 ml, respectively, in nonpregnant women, decrease to mean values of 0.6 mg/100 ml and 9 mg/100 ml in pregnant women. Near term, a 15 to 20% decrement in glomerular filtration rate (GFR) occurs, which affects serum creatinine minimally. Values of creatinine of 0.9 mg/100 ml and BUN of 14 mg/100 ml, which are acceptable in nonpregnant women, are suspect in pregnancy. However, caution is necessary when one is assessing renal function by serum creatinine/inulin clearance normally falling between 1.1 and 1.2. As renal disease progresses, a greater portion of urinary creatinine is formed due to secretion (clearance ratios rising to 1.4 to 1.6 when serum creatinine is 1.4). Therefore, the glomerular filtration may be overestimated by 50%. When preconception serum creatinine and BUN exceed 3 mg/100 ml and 30 mg/100 ml, normal pregnancy is unusual, but successes have been documented in women with moderate-to-severe renal disease, including some treated with dialysis.
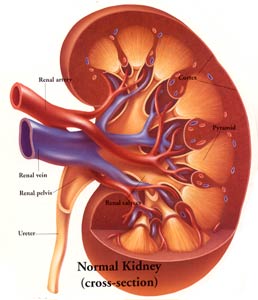
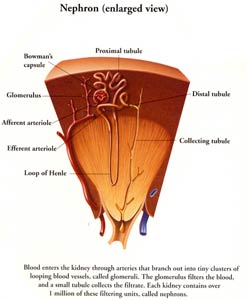
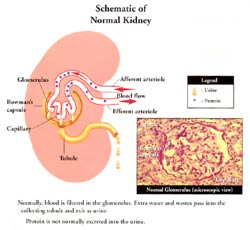
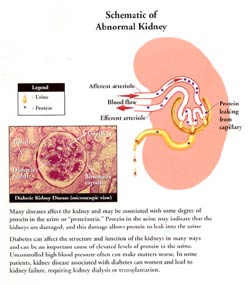
Protein in the urine is also a very important part of the evaluation process of a patient's kidney function and especially so in pregnancy, as we will discuss later. To understand the importance of protein in the urine a little background basics is needed. Each kidney is made up of about 1 million microscopic filtering packets (glomeruli). The purpose of these filtering packets is to filter out the bad stuff and leave the good stuff like protein (building blocks of our muscles) in the blood. Because we have so many of these filtering packets and our lab tests are so sensitive we can actually measure the normal micro amounts of protein that a normal patient spills. A normal person can spill up to 20 mg of albumin (special protein we test the urine for) in a 24 hour urine collection. Some kidney diseases damage these filtering packets which then become like a sieve and cause leakage of excess albumin in the urine. Depending on the disease and the severity of protein spillage can be mild, moderate or severe. Therefore, checking for protein spillage is very important in the evaluation of patient's kidney status. In pregnancy, patients are at risk for increase protein leakage and often it can be the earliest sign of kidney disease in pregnancy.
Hypertension (HTN) in Pregnancy:
HTN occurring as part of pregnancy is relatively common occurring in 12 to 22% of all pregnancies.
HTN in pregnancy can be broadly separated into three categories:
- Pre-existing HTN (chronic HTN)
- Pre-Eclampsia
- Pre-Eclampsia superimposed on Chronic HTN
- Gestational HTN
- Chronic HTN by definition either pre-dated pregnancy or had its onset prior to 20th week of pregnancy. Parameter used are a systolic BP >140 or diastolic BP >90.
(These topics are covered in detail in separate chapters on this web site in Obstetrics Section; please visit this information)
Chronic Hypertension in Pregnancy
Infection of the Urinary Tract:
This chapter is discussed in detail on this web site in Uro/gynecology section. The readers are advised to click on the link to get to the chapter directly.
KIDNEY FAILURE:
The Basics of Kidney Function:
As mentioned previously the main function of the kidney is to clean the blood of the impurities that naturally build up everyday in the body. We can get a rough idea on how well the kidneys are functioning by measuring blood levels of certain molecules that build-up when the kidneys are not functioning at 100% capacity. The blood tests for creatinine (Cr) and blood urea nitrogen (BUN) are our best blood markers for evaluating kidney function. The normal levels for these are as follows:
Cr: 0.4 to 1.4 mg/dl
BUN:10 to 20mg/dl
If the blood levels are above the normal range this often suggests that the patient has impaired renal function. Higher the levels; worse the kidney function.
A better way of measuring the kidney function is to collect a 24 hour urine sample and measure both the urine and blood for these levels and from that calculate the kidney function (Creatinine clearance: Cr Cl). Worse the kidney functions; lower the CrCl.
In pregnancy the blood levels for BUN and Cr tend to be lower because the kidney function is often super-normal in the pregnancy state. Similarly the CrCl during pregnancy tends to be higher than normal during pregnancy.
Patients with kidney dysfunction (i.e. Renal Failure) are typically identified by the increased blood levels of Cr and BUN on routine blood lab testing. By definition we separate kidney failure into ACUTE vs. CHRONIC (see below).
Acute Renal Failure (ARF):
Acute renal failure is defined as the relatively rapid progressive loss of kidney function occurring over a relatively short period of time (days to weeks). One can detect this by lab testing which shows a steady increase in the creatinine (Cr) on repeat testing over the short time period. This happens usually in one of the following clinical situations:
- Acute illness wherein the patient has become seriously ill and usually multiple organ systems have become acutely injured. Examples of this include: severe infection/ trauma/or blood loss wherein the patient's blood pressure becomes very low and the normal circulation to the kidneys is dramatically reduced causing ARF.
- Acute obstruction of the ureters or urethra thus not allowing urine to flow out of the body. This causes back-pressure to the kidneys and can lead to ARF.
- Acute inflammation to the kidneys themselves causing acute dysfunction of the kidneys. This can occur in unusual diseases that attack the kidneys themselves.
During pregnancy or postpartum one can see on rare occasions ARF from any of the above situations. These cases are often very serious and require immediate hospitalization and appropriate medical care by a team of doctors including the nephrologists. Idiopathic postpartum renal failure is also called postpartum malignant nephrosclerosis, irreversible renal postpartum renal failure, and postpartum hemolytic uremic syndrome (HUS). It is rare and frequently fatal syndrome, characterized by the onset of renal failure 3 to 10 weeks into the puerperium after the patient has had an uneventful pregnancy and delivery. The patient develops marked azotemia and severe hypertension and frequently associated with hemolytic anemia and disseminated intravascular coagulation (DIC).
Chronic Renal Failure (CRF):
CRF is by definition distinguished from ARF by the fact that the patient has had loss of kidney function over a more prolonged period of time (more then 3 months and often a process that has been going on for years.
Depending on the severity of chronic damage to the kidneys we separate patients into the following broad categories:
Mild |
60 - 80% of normal function |
Moderate |
30 - 60% |
Severe |
15 - 29% |
End stage Renal Disease |
< 15 % (these patients require renal replacement therapy: Hemodialysis; Peritoneal Dialysis or Kidney Transplantation) |
Patients with CRF need to be thoroughly evaluated by a nephrologist to determine the following information:
Measure the severity of kidney dysfunction (blood work and usually a 24 hour urine test)
Attempt to determine the cause of the CRF (again this requires history and physical exam along with blood and urine testing along with imaging studies of the kidney)
Treatment to delay the progression of the loss of kidney function or possibly arrest the progression. This usually requires aggressive *blood pressure (BP) control and sugar control in diabetic patients. Dietary changes including a moderate restricted protein diet and avoiding potentially kidney damaging medications such as commonly used anti-inflammatory medications.
*The preferred blood pressure (BP) medications used in most patients with CRF includes a class of medications called angiotensin converting inhibitors (ACE-I) and/or angiotensin receptor blockers (ARB). These classes of BP meds provide added kidney protection more so than other BP medications. Unfortunately these medications are CONTRAINDICATED during pregnancy because of their high risk of causing fetal malformations. Patients who are taking these medications and become pregnant must come off these medications immediately and alert their physicians right away. Most studies have shown that the harm from these medications occurs if the medication is continued after the first trimester (after the 13th week).
Pregnancy in Patients with Chronic Renal Failure (CRF):
Can women with CRF get pregnant?
The more severe the degree of CRF the harder it is for the woman to get pregnant. For example women on dialysis only rarely can get pregnant. If they do get pregnant there is high likelihood of miscarriage. The patient requires a team approach between the obstetrician and the nephrologists. There have been cases of women on dialysis during pregnancy going on to delivery but there is a high risk of prematurity and low birth weight in the newborn in these cases.
Antenatal Strategy and Decision-Making: For a successful outcome, scrupulous attention must be paid to blood pressure control, fluid balance, increased hours of dialysis, and provision of good nutrition. The planning of dialysis strategy should have seven aims:
- Maintain BUN < 80 mg/100ml; some would suggest lower, e.g. <50 mg/100ml. Intrauterine death is more likely if levels are much in excess of 80 mg/100 ml, but success has been achieved despite levels of 100 mg/100ml for many weeks.
- Avoid hypotension during dialysis, which could be damaging to the fetus. In late pregnancy the gravid uterus and the supine posture may aggravate this by decreasing venous return.
- Ensure good control of blood pressure.
- Ensure minimal fluctuations in fluid balance and limit volume changes.
- Scrutinize carefully for preterm labor, as dialysis and uterine contractions are associated.
- Watch calcium levels closely and avoid hypercalcemia.
- Limit interdialysis weight gain to about 1 kg until late pregnancy. Also after mid-pregnancy, the classic 0.5 kg/week weight gain should be taken into account when considering dry weight. This should mean a 50% increase in hours and frequency of dialysis. Frequent dialysis renders dietary management and control of weight gain much faster.
Nutrition: despite more frequent dialysis, relatively free dietary intake should be discouraged. A daily oral intake of 70 gm protein, 1,500 mg calcium, 50 mM potassium and 80 mM sodium is advised, with supplements of dialyzable vitamins. Vitamin D supplements can be difficult to judge in patients who have had parathroidectomy. In addition, the placenta produces hydroxyvitamin D, one reason why oral supplementation may have to be curtailed. All this poses risks for fetal nutrition, plus the fact that the exact impact on the uremic environment is difficult to access. The use of parenteral nutrition supplementation in pregnancy in these gravidas has been advocated.
Anemia: patients with severe renal insufficiency are usually anemic. This anemia is usually aggravated further in pregnancy; therefore, blood transfusion may be needed, especially before delivery. Caution is necessary because transfusion may exacerbate hypertension and impair the ability to control circulatory overload, even with extra dialysis. Fluctuations in blood volume can be minimized if packed red cells are transfused during dialysis. Recently rHuEpo has been used in pregnancy without ill effect. It does not have significant transplacental effects. Unnecessary blood sampling should be avoided in the face of anemia and lack of venipunture sites. The protocol for various tests usually performed in a particular unit should be followed strictly, with no more blood removed per venipunture than is absolutely necessary.
Fetal Surveillance and Timing of delivery: cesarean section should be necessary only for purely obstetric reasons. It could be necessary only for purely obstetric reasons. It could be argued; however, that elective cesarean section in all cases would minimize potential problems during labor. In fact, preterm labor is generally the rule and may commence during hemodialysis. The role of cesarean section in this situation needs to be carefully considered.
Does CRF place the fetus at risk?
There are multiple studies that have documented their results in women with CRF who become pregnant. They report their results in pregnant women with varying degrees of CRF and only included those pregnant women who made it past the first trimester. The results show that the higher the Cr (i.e. the more advanced the patients CRF) at time of conception the higher the risk of fetal loss. Interestingly the studies show that the fetal loss is less now then it was in the past. For example:
Fetal loss before 1984: 35%
Fetal loss after 1984: 9%
This is by no means an accurate risk assessment for risk of fetal loss for pregnant women with CRF because it does not take into account the severity of CRF at time of conception. As noted previously the more severe the CRF; higher the risk of fetal loss!
Does CRF place the mother at risk?
There is a marked increase in the risk of superimposed preeclampsia in women with CRF who become pregnant. (65 to 80% develop preeclampsia).
In women with CRF who become pregnant, there is a high risk of irreversible worsening of renal disease as a consequence of the pregnancy. It is generally accepted that if the Cr is greater than 2.0mg/ml the risk of incurring irreversible accelerated loss of renal function in the woman is high. Higher the level of Cr (above 2.0mg/ml); greater is the risk of bad outcome.
Can women who have a kidney transplant get pregnant?
Yes indeed, the transplant woman can get pregnant. The risk to the fetus is dependent on how well the transplant kidney is functioning. The standard immunosuppressive drugs (Cyclosporin and azathioprine) are not associated with increases in fetal abnormalities.
It has been noted that a longer interval between transplant and pregnancy is associated with decreased risk of low birth weigh and prematurity. In general it is often recommended, to wait for two years after transplant before considering pregnancy.
Counseling and Early Pregnancy Assessment:
A woman should be counseled on the various treatments for renal failure and the potential for optimal rehabilitation. Information regarding potential reproductive capacity must be included. Even after transplantation, stress will still be a major factor in everyday life, which will always have a "baseline of uncertainty". Couples who want a child should be encouraged to discuss all the implications, including the harsh realities of maternal prospects of survival.
Preconception guidelines:
Individual centers have their own specific guidelines, in most; a wait of 18 months to 2 years post-transplant is advised. This has turned out to be good advice because, by then, the patient will have recovered from the major surgery and immunosuppression will be at maintenance levels. Also, if function is well maintained at 24 months, there is a high probability of allograft survival at 5 years. A suitable guideline is given here, but the criteria are only relative:
- Good general health about 2 years since transplantation.
- Stature compatible with good obstetric outcome.
- No or minimal proteinuria
- Absence of hypertension
- No evidence of graft rejection
- Absence of pelvicalyceal distension on a recent intravenous urogram
- Stable renal function with plasma creatinine of 2 mg/100 ml or less (preferably less than 1.5 mg/100 ml).
- Drug therapy reduced to maintenance levels: prednisone 15 mg/day or less, and azathioprine 2 mg/kg body weight/day or less. Safe doses of cyclosporine-A, have not yet been established because of limited clinical experience, but 5 mg/kg body weight per day or less is quoted anecdotally.
Ectopic Pregnancy: It occurs in at least 0.5% of all conceptions. The diagnosis can be difficult because irregular bleeding and amenorrhea accompany deteriorating renal function or even an intrauterine pregnancy. Patients may be at higher risk of ectopic pregnancy because of pelvic adhesions due to previous urologic surgery, peritoneal dialysis, pelvic inflammatory disease, or overzealous use of intrauterine contraceptive devices. The main clinical problem is that symptoms secondary to genuine pelvic pathology are erroneously attributed to the transplant.
What effect does pregnancy have on the transplanted Kidney?
It appears that pregnancy itself does not adversely affect the transplanted kidney as long as the kidney is functioning well at time of conception. If the transplant kidney is not functioning well (i.e. CRF) then the risk of accelerating the loss of renal function with pregnancy is similar to that seen in patients with CRF.
Summary:
In general, prognosis is good if renal dysfunction is minimal and hypertension is absent. Pregnancy in women on dialysis can be excessively complicated. Increased frequency and duration of dialysis are needed. There is high fetal wastage at all stages of pregnancy. In the absence of severe maternal problems, the hazards of pregnancy in renal transplant patients are minimal, and successful obstetric outcome is the rule. Acute obstetric renal failure can occur in women with previously healthy kidneys. Pathology peculiar to pregnancy must always be considered.
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com