Рекомендации по уходу перед анестезией для гинекологических пациентов
WHEC практики Бюллетень и клинических управления Руководство для медицинских работников. Образования гранта, предоставленного здоровья женщин-образовательный центр (WHEC).
One of the most important concepts championed in enhanced recovery after surgery (ERAS) pathways is that all staff involved in perioperative care must work together as a single team. In the past, best practices for perioperative management have been based on as much as dogma as science. The creation of optimized perioperative pathways, known as enhanced recovery after surgery, has been shown to simultaneously improve patient outcomes and reduce cost. When possible, we have relied on randomized trials, meta-analyses, and systematic reviews to support our recommendations. In some instances, we have drawn from the general and colorectal surgery literature if evidence in gynecologic surgery is limited or of poor quality. In particular, hospital systems should aim to adhere to antibiotic and thromboembolic prophylaxis for 100% of patients.
The purpose of this review is to assess interventions (and omission of interventions) that should be considered by every surgical team to optimize preanesthesia care. This includes patient education, properly managing existing medical comorbidities, optimizing nutrition, and the use of medications before incision that have been shown to reduce surgical stress, opioid requirements, and postoperative complications. Anesthesia techniques, the use of adjunct medications administered after the incision, and postoperative management are beyond the scope of this review. We have discussed these topics in different reviews in this educational program.
Preoperative Counseling
Patient management is a key element to achieving excellent surgical outcomes and begins with the initial surgical consultation (1). One randomized trial compared written and verbal preoperative information in patients undergoing hysterectomy and bilateral salpingo-oophorectomy for endometrial cancer. Patients who received written information has significantly shorter length of stay, less pain, and less need for pain medications (2). Patients frequently have anxiety over the unknown, loss of control, and fear of pain and complications. Counseling has been shown to reduce anxiety and may play an important part in managing analgesia (3). A patient diary with goals for recovery such as oral intake, regular pain relief, removal of drains and catheters, and goals for mobilization may be used to accelerate recovery and guide patient's pathway during their hospital stay. An expected discharge date and arrangements for placement to a skilled nursing facility, if needed, is best planned before admission. Failure to do so may result in increased length of hospital stay with resulting higher costs of care.
Prehabilitation
Prehabilitation is a term used to describe the process of improving patients' physical and nutritional state before surgery and does not include optimization of medical conditions (e.g. heart failure, coronary disease). Elderly or frail patients are at increased risk of perioperative complications and prolonged recovery (4). It is therefore logical to expect that aerobic and resistance exercise combined with nutritional protein supplementation to build muscle mass should improve physical reserve and toleration of surgery. Optimal perioperative nutrition is important to improve tissue healing and reduce complications and infections. Patients who are nutritionally impaired have three times the risk of postoperative complications and five times the risk of mortality, in addition to prolonged length of stay, higher readmission rates, and higher costs. (5).
A useful screening tool has been published by the Perioperative Quality Initiative group to identify those risk patients at risk (6). The use of whey-protein or propriety protein drinks is beneficial, but the addition of fish oils and arginine, referred to as immunonutrition, remains controversial. At least seven days of perioperative supplementation is required for benefit (7). See figure 1 below.
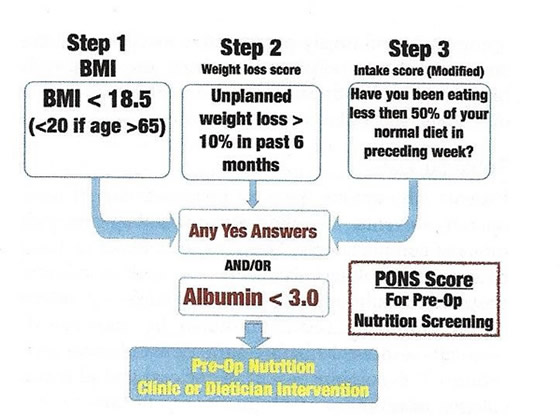
Figure 1. Screening tool for nutritional impairment.
Cardiopulmonary exercise testing a means of measuring aerobic fitness and peak oxygen delivery to monitor progress in fitness programs and interventions before surgery to assist with risk stratification (8). One recent study that aimed to improve perioperative aerobic exercise performance in high-risk patients reduced postoperative complications by 51% (9). Another investigation combining aerobic and resistance muscle training with whey-protein supplementation did not reduce complication rates but did shorten the interval from surgery to return of baseline functional status (10).
Although promising, a key limitation of prehabilitation is the time-schedule required to achieve a beneficial effect. Although prehabilitation may be beneficial for patients undergoing elective surgery or requiring neo-adjuvant chemotherapy, its usefulness is limited for patients in need of surgery in a short time-frame. Patients with poor preoperative aerobic capacity or frailty are most likely to obtain benefit from prehabilitation. A structured and supervised program is mandatory to reduce beneficial results.
Carbohydrate Loading and Preoperative Nutrition
"Nil by mouth" is among the oldest and most common dogmas known in surgery. The avoidance of solid food for 6 hours before surgery to avoid aspiration is rational, but the avoidance of fluid is not. Dehydration and nil-by-mouth increase the incidence of anxiety, stress, hunger, and postoperative nausea and vomiting. In fact, guidelines from the American Society of Anesthesiologists allow clear liquids up to 2 hours before induction of anesthesia (11). Nevertheless, a large proportion of patients undergo surgical procedures in a stressed, dehydrated state that is often exacerbated by delays the morning of surgery. Although the evidence based for carbohydrate loading is currently extrapolated from studies in intra-abdominal and colorectal surgery, carbohydrate drinks are a recommended element of enhanced recovery pathways, including for gynecologic surgery, to ensure the patient is hydrated and has adequate energy stores (12).
Various forms of carbohydrate drinks have been advocated, including simple juices and maltodextrin solutions (polysaccharides), which should be consumed the evening before and up to 2 hours before anesthesia; written instructions should be provided. These drinks have low osmolarity, are safely emptied from the stomach, and do not increase the risk of aspiration. In addition to be the first step on a path to maintain intravascular euvolemia and reduce fluid shifts, carbohydrate loading has been shown to improve insulin sensitivity, reduce catabolism, and improve grip strength after major surgery (13).
Theoretically, the improvement in perioperative insulin sensitivity seen with carbohydrate loading should benefit patients with type 2 diabetes mellitus but may result in a small rise in blood glucose, requiring small amounts of corrective insulin sensitivity improved by carbohydrate loading, so they would benefit only from the hydration effect. High-quality data to guide optimal care in patients with diabetes are not available, but, together with concerns about delays in gastric emptying, water may be substituted for a carbohydrate drink in these patients.
Medical Conditions Increasing Perioperative Risks
Perioperative risk and readiness for surgery should be assessed by the anesthesia team. For most patients this is safely accomplished in the morning of surgery when the team meets with the patient to determine the anesthesia plan. However, specific medical conditions pose a particular challenge and suboptimal preparedness before surgery has been shown to increase perioperative morbidity and mortality.
Tobacco use: Patients who smoke have an increased risk of perioperative events, including wound healing and pulmonary complications. They are also likely to have concurrent smoking-related diseases such as chronic obstructive pulmonary disease or coronary artery disease. Smoking cessation should be encouraged, optimally 4-8 weeks before surgery for elective procedures (14). A combination of behavioral and pharmacologic intervention with nicotine substitution are most efficacious for successful cessation. After cessation, a period of bronchial hyperactivity may occur which is best treated with inhaled steroids and bronchodilators. Nicotine patches may be beneficial to reduce the risk of withdrawal during the perioperative period. To reduce the risk of postoperative respiratory complications, patients should receive instruction on the use of incentive spirometer before admission.
Alcohol Use Disorder: Patients should be screened to assess their weekly alcohol intake in units and encouraged to stop or reduce their alcohol intake before surgery. Even modest intake (more than two drinks per day) has been shown to increase the risk of infection (15). Patients with excessive intake are at increased risk of delirium, withdrawal, and postoperative complications. The Alcohol Use Disorder Identification Test Consumption Questionnaire scoring test may be used to identify those at higher risk. Those with a score higher than 5 are at higher risk of complications, and a score of 9 or higher predicts a longer length of stay.
Opioid Dependence: Investigations have shown that approximately 6% of patients will develop new persistent opioid use postoperatively; the rate is as high as 21% for those who require chemotherapy after surgery (16). This has led to efforts to reduce and standardize opioid prescribing in the postoperative period.
A particularly important consideration is the treatment of patients on preoperative buprenorphine, a relatively new mixed opioid agonist-antagonist unfamiliar to many surgeons. Buprenorphine is a partial mu-agonist and a high-affinity antagonist at the kappa receptor, conferring the advantage of low rates of side effects, such as respiratory depression, nausea, constipation, and physical dependence. Furthermore, buprenorphine binds with high affinity to these receptors, with a half-life of 37 hours, and may treat opioid-induced hyperalgesia and depression. These characteristics make it very effective for the treatment of opioid use disorder and withdrawal but also prevent other opioids from binding, thereby reducing their efficacy. The analgesic ceiling occurs at 24-32 mg, such that unlike other opioids, increasing doses of buprenorphine may not be effective in treating progressive pain. Recognizing that the pharmacodynamics create unique challenges for postoperative pain control, all patients using buprenorphine should be evaluated by a pain specialist for optimal management.
Options for these patients include continuing buprenorphine through perioperative period, or discontinuation before surgery (17). Continuing buprenorphine may cause significant difficulties with post-operative pain control, requiring extremely high doses of opioid, and so is the best choice for patients undergoing minor procedures with only mild pain expected postoperatively. Discontinuation may be the best option if significant pain is expected, but it must occur at least 3 – 7 days postoperatively for other opioids to be effective, given its long half-life. Discontinuation is also associated with a higher risk of relapse, may be associated with acute withdrawal owing to its antagonistic effects.
Advanced Age: Older individuals tend to have a higher risk for perioperative morbidity, a function of comorbid conditions rather than older age alone (18). The American Geriatrics Society in collaboration with the American College of Surgeons (ACS) National Surgical Quality Improvement Program published a systematic review in which they recommended that routine preoperative screening tests should not be performed in patients older than 65 years with the exception of hemoglobin, renal function and albumin, and the other preoperative diagnostic tests should be ordered only on the basis of individualized risk factors and existing comorbidities.
Cardiovascular Disease: Patients with cardiovascular diseases including hypertension, heart failure, arrhythmias, valvular heart disease, and coronary artery disease have a higher risk for perioperative cardiovascular complications. The American College of Cardiology jointly with the American Heart Association Task Force conducted an extensive review of the literature and published a guideline document detailing appropriate perioperative cardiovascular evaluation and treatment of patients undergoing non-cardiac surgery (19).
Hypertension is one of the most commonly encountered cardiovascular diseases present preoperatively. If the preoperative blood pressure is unknown, elective surgery may still be safely performed with blood pressures less than 180/110 mm Hg in the preoperative clinic or the day of surgery (20). For patients who have undergone a percutaneous coronary intervention with stenting, the timing of elective non-cardiac surgery is dependent on the risk of premature discontinuation of dual antiplatelet therapy compared with the consequences of delaying surgery. Given the higher risk for stent thrombosis and adverse cardiac events after premature discontinuation of dual antiplatelet therapy after placement of bare metal or drug-eluting stents, non-urgent non-cardiac surgery should be deferred for 6 months (19). However, if the risk of delaying surgery outweigh the risks of adverse cardiac outcomes including stent thrombosis, non-urgent non-cardiac surgery may be considered as early as 3 months recognizing that stent-related adverse outcomes appear to plateau at 3 – 6 months. Consultation with cardiologist is recommended to definitely identify the type of stent placed and assist with risk assessment.
Patients on chronic beta-blockers should remain on them in the perioperative period (19). If preoperative initiation of beta-blockers is considered with the intent of reducing short-term perioperative risk for myocardial ischemia, consultation with cardiologist is required to weigh risks and benefits. Conversely, beta-blockers should not be initiated in the perioperative period for long-term indications. Doing so, is associated with an elevated risk for perioperative stroke, which outweighs the uncertain benefit of reduction of perioperative cardiac events. This effect is pronounced when initiated the day of surgery (19).
Surgeons should be familiar with condition severe aortic valve stenosis or any aortic valve stenosis with symptoms (angina, syncope, heart failure), severe mitral valve stenosis, severe hypertrophic obstructive cardiomyopathy, pulmonary hypertension, and severe right heart failure. In addition, as treatment of congenital cardiac anomalies has improved, we will continue to see an increasing number of adult women with these conditions who require gynecologic surgery. Physiologic goals for patients with these diagnoses are very specific and differ slightly from the usual. Therefore, such patients should be evaluated by anesthesiology preoperatively and may require the attendance of a cardiac anesthesiologist.
Preoperative Anemia: Preoperative anemia is an important risk factor for suboptimal surgical outcomes. In a European study of nearly 40,000 surgical patients, more than 30% of women were anemic preoperatively (21). A hemoglobin of less than 10.5 g/dL was associated with higher mortality and other complications, in addition to prolonged length of hospital stay. 51% of women are iron deficient, even with a hemoglobin higher than the World Health Organization (WHO) definition of 12 g/dL, owing to menstruation or dietary factors. Optimal oncologic practice is to avoid perioperative blood transfusion, and preoperative transfusion has not been shown to be of benefit unless values are less than 7 g/dL (22). An underused option to increase preoperative hemoglobin for elective surgery is the administration of intravenous (IV) iron. Newer IV iron preparations have a low incidence of adverse events and can be given as an outpatient in visits of less than 2 hours. In one investigation, anemic patients who received IV iron demonstrated a mean rise in hemoglobulin of 1.55 g/dL over a 2-week period (vs a 0.5-g/dL rise for oral iron) (23). The urgency of surgery and rate of blood loss should be considered when determining when to use IV iron or red blood cell transfusion.
Cerebrovascular Disease: Patients with a recent cerebrovascular event are at increased risk of adverse postoperative outcomes, especially within the first 9 months. After 9 months, patients remain at a low, yet somewhat elevated risk based on a Danish nationwide cohort study (24). For this reason, elective surgery after a recent stroke or transient ischemic attack should be carefully considered and potentially deferred with a focus on first addressing the atherosclerotic artery disease.
Pulmonary Disease and Obstructive Sleep Apnea: Evaluation of preoperative pulmonary risk should be part of any standard preoperative medical evaluation. The American Society of Anesthesiologists Task Force, the Society of Anesthesia and Sleep Medicine, and the American College of Physicians have published guidelines on risk assessment and strategies to reduce perioperative pulmonary complications in this setting (25).
Diabetes: Unrecognized hyperglycemia has been shown to increase the risk of adverse perioperative outcomes compared with known diabetes. Preoperative assessment of glycemic control with hemoglobin A1c (Hb A1c) and random blood sugar measurements in patients at high risk for or with known diabetes is important to risk stratify patients for postoperative wound infections. The Endocrine Society and the American Diabetes Association support glycemic goals between 110 and 180 mg/dL for noncritically ill hospitalized patients, including within the perioperative period (26). Patients with diabetes have a higher risk or postoperative infections morbidity, but also cardiovascular morbidity and overall mortality owing to coexisting comorbidities including cardiovascular disease, hypertension, obesity, chronic kidney disease, cerebrovascular disease, and autonomic neuropathy.
Obesity: It poses a particular challenge perioperatively. It is associated with a higher risk of conversion from laparoscopy to laparotomy and is frequently associated with other conditions that increase perioperative risk including diabetes, hypertension, heart disease, obstructive sleep apnea, difficult airway management, and venous thromboembolism. In addition to preanesthesia evaluation, assessment of the obese surgical patient should be directed toward management of these conditions. In a guideline document on perioperative care, it is recommended that patients with obesity class III (body mass index [calculated as weight in kilograms divided by height in meters squared] 40 or greater) have a formal consultation with the anesthesiology department as part of their preoperative evaluation (27). However, high quality evidence of how to properly select obese patients who would benefit from such consultation is lacking.
Renal and Hepatic Dysfunction: Chronic kidney and liver conditions significantly increase perioperative morbidity and mortality. Outcomes vary widely based on severity of disease and require and individualized approach. Multidisciplinary management with nephrologists, hepatologists, and transplant surgeons is obligatory to assess for severity of preexisting disease and surgical risk, which may vary from unacceptable to minimally increased (28).
Bowel Preparation
Limited high-quality data exist regarding the use of bowel preparation in gynecologic surgery, particularly for patients undergoing minimally invasive gynecologic surgery. In a recent systematic review conducted for the Agency for Healthcare Research and Quality (AHRQ) Safety Program for improving surgical care and recovery, the authors identified one systematic review, two meta-analyses, and two randomized controlled trials published after the systematic review on the use of bowel preparation for patients undergoing gynecologic laparoscopic or vaginal surgery for benign indications (29). All studies concluded that use of bowel preparation did not offer benefit, including ease of surgery or bowel handling. Use of bowel preparation before minimally gynecologic surgery is thus not recommended according to existing societal guidelines. Given the lack of data in the gynecologic surgical literature, data often are extrapolated from the colorectal literature.
Although there are no randomized trials directly comparing oral antibiotics with mechanical preparation plus oral antibiotics, or with no bowel preparation, data from retrospective studies suggest that oral antibiotics alone may be as efficacious as the combined regimen in reducing infectious morbidity (30). Importantly, studies reporting outcomes of well-established enhanced recovery pathways as well as comprehensive surgical site infection reduction bundles in which bowel preparation was entirely omitted in gynecologic surgery (with or without bowel resection) showed that rates of infection and anastomotic leak rates were not negatively affected. In fact, surgical site infection rates as low as 2.4% have been reported for patients undergoing colonic resection for gynecologic malignancy (31). Although societal guidelines discourage the use of the combined regimen before elective colorectal surgery, it appears reasonable to consider omitting bowel preparation before gynecologic surgery, even when planning a bowel resection, in the setting of established ERAS pathways or within a surgical site infection reduction bundle. However, if there is desire for bowel preparation, oral antibiotics alone or the combination should be used. This practice is in agreement with existing societal guidelines (31).
Preoperative Venous Thromboembolism Prophylaxis
Use of prophylaxis in the preoperative setting may help reduce the overall incidence of venous thromboembolism recognizing that thrombus formation may occur as early as at the time of induction of anesthesia. Abdominal and pelvic surgery carries a high risk for perioperative thromboembolism. Venous thromboembolism risk is also heavily influenced by the indication for surgery (benign vs malignant). In this study the overall incidence of clinical venous thromboembolism was 0 – 2% in the population undergoing gynecologic surgery for benign indications, with no events identified in the population undergoing laparoscopic surgery for benign conditions (32). However, the rate is as high as 35% in the gynecologic oncology population without prophylaxis (32). This illustrates the need for risk stratification.
The ERAS Society, the American College of Obstetricians and Gynecologists (ACOG), the American College of Chest Physicians, and the American Society of Clinical Oncology support the use of intermittent pneumatic compression alone before minimally invasive gynecologic surgery and the dual use of intermittent compression and chemoprophylaxis with either unfractionated heparin or low molecular weight heparin before major oncologic gynecologic surgery as preoperative prophylaxis.
Preoperative Antibiotics Prophylaxis
The American Society of Health-System Pharmacists, jointly with the Infectious Diseases Society of America, the Surgical Infection Society, and the Society for Healthcare Epidemiology of America, as well as ACOG have published systematic reviews and detailed guidelines on antibiotic prophylaxis before gynecologic surgery (33). With regards to the choice of antibiotic, first-generation cephalosporins, primarily cefazolin, have been shown to be at least as effective as second- and third-generation cephalosporins, primarily cefazolin, have been shown to be at least as effective as second- and third- generation cephalosporins in gynecologic surgery. For patients with a penicillin allergy, alternative regimens such as clindamycin, or metronidazole plus gentamicin, or aztreonam are recommended (33). However, a recent study by the Michigan Surgical Quality Collaborative showed that women receiving non-first-line antibiotics had a 1.7 to 2.0 increase in the risk of any surgical site infection compared with those receiving first-line antibiotics, highlighting the importance of skin testing to determine whether a true penicillin allergy exists (34).
Important determinants of efficacy include appropriate timing of administration and dosing. Although antibiotics were initially recommended to be given "at induction of anesthesia," updated guidelines recommend most antibiotics to be administered within 60 minutes before incision with agents such as fluoroquinolones and vancomycin within 120 minutes before incision given longer infusion times (33). Dosage adjustments based on body weight should be made to reach appropriate tissue levels. Specifically, for cefazolin dosing, guidelines have been simplified to 2 g for adult patients weighing less than 120 kg and 3 g for those weighing more than 120 kg (33). Additional intraoperative doses should be given based on the duration of surgery and estimated blood loss. Intraoperative antibiotics should be re-dosed based on the time of incision after two half-lives of the drug (4 hours for cefazolin). An additional dose is recommended of cefazolin should be given when blood loss is greater than 1,500 mL.
Pharmacologic Adjuncts
The use of preemptive pharmacologic agents may confer greater benefit to patients with administered before incision rather than after. Purported advantages include reductions in nausea and vomiting, opioid requirements through a modulation of the pain response, surgical stress, and inflammation. Such non-opioid alternatives are especially useful for patients who have used people opioids preoperatively, but they are nevertheless indicated for most patients undergoing major surgery.
A common cocktail used in many ERAS pathways includes administration of oral acetaminophen, celecoxib (COX-2 inhibitor), and gabapentin just before induction of anesthesia. Gabapentin is a third-generation antiepileptic drug with central and peripheral antinociceptive activity. A meta-analysis of more than 3,000 patients undergoing a variety of surgical procedures showed that both COX-2 inhibitors and gabapentin were effective in reducing acute postoperative pain when administered before surgery; in contrast, these effects were not demonstrated for opioids or other non-steroidal anti-inflammatory drugs (35). The authors suggest that a single, 300-mg dose of gabapentin 1-2 hours before incision is optimal, as further improvement was not seen with additional postoperative doses; side effects were similar to placebo.
Glucocorticoids are commonly used antiemetics, but at higher doses confer analgesic effects through inhibition of prostaglandin synthesis, and modulation of the inflammatory response through inhibition of interleukins and tumor necrosis factor-alpha. A review of 24 randomized trials with more than 2,700 patients undergoing a variety of surgical procedures, including laparoscopic hysterectomy, showed that at intermediate doses greater than 0.1% mg/kg, a single dose of dexamethasone effectively reduces pain, opioid consumption, and time to discharge; this effect was more consistent if given preoperatively (36). Improvements in pain compared with placebo were observed both in the first 4 hours and first 24 hours after surgery. Of note, there was no difference in opioid reduction when comparing intermediate-dose with high-dose (0.2 mg/kg and above) dexamethasone. There is no evidence suggesting that intermediate dose dexamethasone increases the risk of wound infection or hyperglycemia.
A randomized trial limited to patients undergoing laparoscopic hysterectomy showed that 15 mg of IV dexamethasone was more effective than 5-mg or 10-mg dosing in reducing opioid use in the first 24 hours after surgery (37). No adverse effects were noted, although patients with diabetes were excluded from the trial.
Implementation of Evidence-based Decision-making
Evidence-based decision-making should replace the often-heard justification, "This is how I have always done it." The use of auditing has been effective in ensuring compliance with recommended perioperative interventions and improved outcomes (38). Two mechanisms for implementation and auditing include the ERAS Society's Enhanced Recovery Interactive Audit System and the upcoming Safety Program for Improving Surgical Care and Recovery sponsored by the AHRQ in partnership with the ACS and the Armstrong Institute at Johns Hopkins. Such audits may also be augmented by continuous assessment of surgical outcomes through the use of the ACS National Surgical Quality Improvement Program.
Just as surgeons will continue to innovate and develop novel interventions to more effectively treat disease, surgeons should partner with anesthesiologists and other care providers to develop best perioperative practices to optimize recovery. Our goal should be to implement as many of these interventions as possible, to as many patients as possible. The use of common order sets are now commonplace in electronic health records and facilitate standardized implementation throughout surgical areas and even entire health systems. This strategy diminishes variation in perioperative management, reducing confusion among other members of the surgical team and decreasing variation in outcomes between surgeons. In particular, hospital systems should aim to adhere to antibiotic and thromboembolic prophylaxis for 100% of patients.
Summary
There are a number of interventions that have been shown to optimize preanesthesia care for patients undergoing gynecologic surgery. Although some elements will be more effective than others, optimizing as many aspects as possible may very well have synergic effects, consistent with recent descriptions of bundling many interventions for optimal outcomes. This subject will continue to evolve as new data are collected. Although few would argue against the value of patient education or optimizing existing medical comorbidities, other topics will benefit from further investigation.
A relative lack of type I data are available to identify the least expensive and most effective means of carbohydrate loading to optimize nutrition, and the timing, duration, and benefits of rehabilitation requires further definition. Although pharmacologic adjunct appear beneficial to diminish physiologic derangements that occur secondary to surgical stress, the most efficacious combination of drugs, as well as optimal dose, timing, and duration of administration has yet to be identified.
References
- Hounsome J, Lee A, Greenhalgh J, et al. A systematic review of information format and timing before scheduled adult surgery for perioperative anxiety. Anesthesia 2017;72:1265-1272
- Angioli R, Plotti F, Capriglione S, et al. The effects of giving patients verbal or written preoperative information in gynecologic oncology surgery: a randomized study and the medical-legal point of view. Eur J Obstet Gynecol Reprod Biol 2014;177:67-71
- Powell R, Scott NW, Manyande A, et al. Psychological preparation and postoperative outcomes for adults undergoing surgery under general anesthesia. The Cochrane Database of Systematic Reviews 2016; Issue 5. Art. No.: CD008646. DOI: 10.1002/14651858. CD008646.pub2
- Carli F, Scheede-Bergdahl C. Prehabilitation to enhance perioperative care. Anesthesiol Clin 2015;33:17-33
- Weimann A, Braga M, Carli F, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr 2017;36:623-650
- Wischmeyer PE, Carli F, Evans DC, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative joint consensus statement on nutrition screening and therapy within a surgical enhanced recovery pathway. Anesth Analg 2018;126:1883-1895
- Scott M. Martindale R. Perioperative nutrition: a high-impact, low-risk, low-cost intervention. Anesth Analg 2018;126:1803-1804
- Richardson K, Levett DZH, Jack S, Grocott MPW. Fit for surgery? Perspectives on preoperative exercise testing and training. Br J Anesth 2017;119(suppl 1):134-143
- Barberan-Garcia A, Ubre M, Roca J, et al. Personalized Prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 2018;267:50-56
- Gillis C, Li C, Lee L, et al. Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology2014;121:937-947
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology 2017;126:376-393
- Nelson G, Altman AD, Nick A, et al. Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations - part I. Gynecol Oncol 2016;140:313-322
- Barazzoni R, Deutz NEP, Biolo G, et al. Carbohydrate and insulin resistance in clinical nutrition: recommendations from the ESPEN expert group. Clin Nutr 2017;36:355-363
- Wong J, Lam DP, Abrishami A, et al. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth 2012;59:268-279
- Shabanzadeh DM, Sorensen LT. Alcohol consumption increases post-operative infections but not mortality: a systematic review and meta-analysis. Surg Infect 2015;16:657-658
- Thiels CA, Ubi DS, Yost KJ, et al. Results of a prospective, multicenter initiative aimed at developing opioid-prescribing guidelines after surgery. Ann Surg 2018;268:457-468
- Anderson TA, Quaye ANA, Ward EN et al. To stop or not to stop, that is the question: acute pain management for the patient on chronic buprenorphine. Anesthesiology 2017;126:1180-1186
- Chow WB, Rosenthal RA, Merkow RP, American College of Surgeons National Surgical Quality Improvement Program, et al. Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg 2012;215:453-466
- Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing non-cardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 2014;64:e77-137
- Hartle A, McCormack T, Carlisle J, et al. The measurement of adult blood pressure and management of hypertension before elective surgery: Joint Guidelines from the Association of Anesthetists of Great Britain and Ireland and the British Hypertension Society. Anesthesia 2016;71:326-337
- Munoz M, Laso-Morales MJ, Gomez-Ramirez S, et al. Pre-operative hemoglobin levels and iron status in a large multicenter cohort of patients undergoing major elective surgery. Anesthesia 2017;72:826-834
- Kotze A, Harris A, Baker C, et al. British committee for standards in hematology guidelines on the identification and management of pre-operative anemia. Br J Haemol 2015;171:322-331
- Keeler BD, Simpson JA, Ng O, et al. Randomized clinical trial of preoperative oral versus intravenous iron in anemic patients with colorectal cancer. Br J Surg 2017;104:214-221
- Jorgensen ME, Torp-Pedersen C, Gislason GH, et al. Time elapsed after ischemic stroke and risk of adverse cardiovascular events and mortality following elective noncardiac surgery. JAMA 2014;312:269-277
- Chung F, Memtsoudis SG, Ramachandran SK, et al. Society of anesthesia and sleep medicine guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg 2016;123:452-473
- Duggan EW, Carlson K, Umpierrez GE. Perioperative hyperglycemia management: an update. Anesthesiology 2017;126:547-560
- Dindo D, Muller MK, Weber M, Clavien PA. Obesity in general elective surgery. Lancet 2003;361:2032-2035
- Mathew A, Devereaux PJ, O'Hare A, et al. Chronic kidney disease and postoperative mortality: a systematic review and meta-analysis. Kidney Int 2008;73:1069-1081
- Dwody SC, Kalogera E, Scott M. Optimizing preanesthesia care for the gynecologic patient. Obstet Gynecol 2019;134:395-408
- Koller SE, Bauer KW, Egleston BL, et al. Comparative effectiveness and risks of bowel preparation before elective colorectal surgery. Ann Surg 2018;267:734-742
- Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg2013;37:259-284
- Rahn DD, Mamik MM, Sanses TV, et al. Venous thromboembolism prophylaxis in gynecologic surgery: a systematic review. Obstet Gynecol 2011;118:1111-1125
- Prevention of infection after gynecologic procedures. ACOG Practice Bulletin No. 195. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131:e172-189
- Uppal S, Harris J, Al-Niami A, et al. Prophylactic antibiotic choice and risk of surgical site infection after hysterectomy. Obstet Gynecol 2016;127:321-329
- Nir RR, Nahman-Averbuch H, Moont R, et al. Preoperative preemptive drug administration for acute postoperative pain: a systematic review and meta-analysis. Eur J Pain 2016;20:1025-1043
- De Oliverira GS Jr, Almeida MD, Benzon HT, et al. Perioperative single dose systematic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology 2011;115:575-588
- Jokela RM, Ahonen JV, Tallgren MK, et al. The effective analgesic dose of dexamethasone after laparoscopic hysterectomy. Anesth Analg 2009;109:607-615
- Bisch SP, Wells T, Gramlich I, et al. Enhanced Recovery After Surgery (ERAS) in gynecologic oncology: system-wide implementation and audit leads to improved value and patient outcomes. Gynecol Oncol 2018;151:117-123
Опубликован: 3 March 2020
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


