Posttraumatic Stress Disorder
WHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC).
Posttraumatic stress disorder (PTSD) is a serious anxiety disorder triggered by the experience of trauma. One in 4 individuals exposed to trauma will develop PTSD. Victims of trauma are frequent users of health care, but screening is rarely done and most sequelae remain undetected. In recent years, it has become evident that PTSD is a major health concern both in United States and worldwide. Unfortunately, it continues to be poorly recognized and not well treated, though long-lasting morbidity results from the disorder. Risk factors for trauma and PTSD are not identical. It is unusual for PTSD to exist in isolation: most commonly one or more Axis I disorders will be found to coexist. Associations between PTSD and common disorders such as depression, anxiety, eating disorders, and alcohol and substance abuse are prevalent.
The purpose to this document is to enhance the understanding of posttraumatic stress disorder (PTSD) and evaluate screening modalities for PTSD. It is a debilitating form of an anxiety disorder triggered by personal experience of serious trauma (eg, sexual abuse or assault, victim of violent crime or severe motor vehicle accident). The course of untreated disease averages more than 5 years and may lead to additional psychiatric comorbidity, including a greatly increased risk of major depression and suicide (1). The medicines to treat PTSD with fewer side effects is a possibility and it remains an intriguing idea, and one that ushers in an era of effective drugs with much less side effects.
Epidemiology:
Epidemiologic studies show that prevalence of trauma and posttraumatic stress disorder (PTSD) is substantial in modern society. Most people will experience a traumatic event at some point in their life, and up to 25% of them will develop the disorder. Demographic and socioeconomic factors also play a role in the risk for exposure to traumatic experiences and subsequent PTSD. Psychiatric history, both personal or in family members, increases the likelihood of being exposed to trauma and of developing PTSD once exposed. Posttraumatic stress disorder (PTSD) has gained increasing recognition since its first formulation as a diagnosis in the Diagnostic and Statistical Manual of Mental disorders, Third Edition (DSM-III).
PTSD rates have frequently been studied in persons exposed to different specific traumas like combat, sexual assault, rape, natural disasters and other extreme events. More recently, the prevalence of PTSD has been assessed in the general population using nationally respective samples, as well as in samples from specific geographic areas. Lifetime prevalence of PTSD rates from surveys of the general adult population range from 1.0% to 9.2% (2). Women are higher risk for PTSD than men. It is also more frequent after certain types of trauma (eg, rape) regardless of the survivor's gender. Norris investigated the frequency and impact of different traumatic events in a southeastern US population. In that study, the author found a prevalence of 7.3% for current (within the past year) PTSD among individuals who had experienced traumas. Looking at prevalence rates of current PTSD in different traumata, the lowest rate was associated with combat (2%) and the highest with sexual assault (14%). The data also showed that a current PTSD diagnosis was more frequent after violent crimes, death, or accidents than after various environmental hazards (7% - 11% vs. 5% - 8%, respectively) (3).
Gender: Risk factors for exposure to trauma and for PTSD in different studies are that, men are at higher risk for traumatic exposure than women. Norris (3) reported that this difference was significant for lifetime (p=0.05) but not past-year frequencies of exposure -73.6% in men vs. 64.8% in women and 19.5% in men vs. 22.4% in women respectively. The 1996 Detroit Area Survey of Trauma showed that men had twice the possibility of women of being exposed to events in which they were at risk (eg, assaultive violence).
Main characteristics of exposure to trauma and PTSD by gender are:
Men: Exposure to trauma - at higher risk than women; more physical assault and other life-threatening situations; parental substance abuse; parental divorce and history of early conduct problem. PTSD risks -- more frequent if history of psychiatric disorder, parental psychiatric disorder; at higher risk if married at the time of trauma; lower education; combat; childhood neglect; physical abuse and sudden unexpected death of a loved one.
Women: Exposure to trauma -- women are at lower risk than men; more sexual assaults and childhood parental neglect. Risk factors include history of affective, anxiety or substance abuse; parental mental illness and substance abuse; parental aggression; lower education, younger age, being married at the time of the trauma or having been married previously. Urban residence and lower income are significant predictors. PTSD risks -- women are at higher risk than men; more frequent if history of psychiatric disorder; parental psychiatric disorder; parental aggression; younger age and prior trauma exposure are significant predictors. Leading trauma, such as, sexual assault, rape, sudden unexpected death of loved one increases the risks.
Race: There is no consistency about which ethnic group is at higher risk for PTSD. It is seen higher among nonwhites although at a statistically non-significant level.
Personality and Psychiatric history: As associated with a variety of psychiatric disorders (eg, obsessive-compulsive disorder, dysthymia, and manic-depressive disorder). It could be predicted by a history of behavioral problems before the age of 15 years (eg, stealing, lying, truancy and vandalism) and that the rate of PTSD increased with the number of behavioral problems. Being abused as a child increases the possibility of developing PTSD. History of previous affective and/or anxiety disorders is a significant predictor of PTSD in both genders. The patients with PTSD are 2.8 times more likely to have history of psychiatric illness in their relatives.
Type of Trauma: Davidson et al (4) noted that the most frequent traumata reported by people who had PTSD were (i) threat or close call, (ii) seeing someone hurt or killed, (iii) physical attack, (iv) accident, and (v) combat. The highest rate of PTSD (80%) is seen in rape cases. Other high probability of PTSD includes combat, childhood neglect, and childhood physical abuse. The lifetime prevalence of exposure to any traumatic situation in general populations has been shown to be as high as 90%. This indicates a high likelihood for every human to become exposed to at least one traumatic event during his or her life span. Moreover, it is quite common to be exposed to more than one trauma and for traumatic situations to reoccur across time. People exposed to traumas like combat or sexual assault and persons exhibiting PTSD related to those traumatic experiences sustain a deleterious impact on their health and their health perceptions. The likelihood of misdiagnosis, non-recognition, and inappropriate treatment remain high for PTSD and leads to a high direct cost of PTSD. There is also an indirect cost that is related to the loss of productivity at work.
Biology of Posttraumatic Stress Disorder (PTSD):
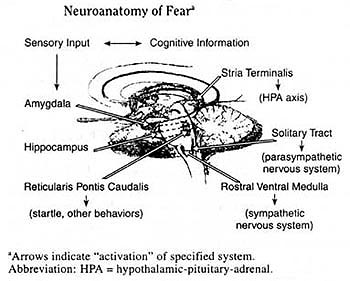
By its very nature the biology of PTSD is fundamentally different form the biology of stress because it describes a process that occurs well after the stress is no longer physically present. Thus, the essential question of the biology of this disorder is one of delineating why there has been a failure of the body to return to its pre-traumatic state. It appears to be less important to consider the actual biology of stress in addressing this issue because PTSD is not an inevitable outcome of stress. More than half of those who develop PTSD also appear to recover from this disorder. The symptoms of PTSD have been conceptualized as resulting from the cascade of biological and psychological responses following the activation of fear-related and other brain systems. Exposure to traumatic stress results in a fear response, which involves the initiation of concurrent and instantaneous biological responses that help assess the level of danger and then organize an appropriate behavioral response. Stress -- particularly acute stress -- results in a dose-dependent increase in both catecholamines and cortisol. The greater the severity of the stressor, the higher the levels of both hormones. The amygdala is the brain organ that serves as the major interface between the sensory experiences, such as the major interface between the sensory experiences, such as seeing an aggressor and perceiving indications of his or her harmful intentions, and the biochemical and behavioral systems that ultimately respond to this information (5). See the Neuro-anatomy pathway below:
To date, several important statements can be made about the biology of PTSD. First, the biology of PTSD does not appear to completely reflect the biological alterations that are observed at the time of the traumatic event. Second, not all of the biological alterations in PTSD reflect similar aspects of the traumatic experiences. Indeed, some biological alterations may be related to the risk for PTSD and actually explain the development of other biological responses. Some alterations may be secondary consequences of the traumatic stress response or may develop in response to PTSD symptoms. Third, the biology of PTSD seems, in many respects, to be different than biological alterations observed in other psychiatric disorders, particularly major depressive disorder. This is particularly interesting since so many symptoms of PTSD are similar to symptoms in major depressive disorders, and trauma survivors frequently meet the diagnostic criteria for both disorders. There are many gaps in our knowledge about the biology of PTSD, largely because we have not, as a field, mapped out developmental changes using prospective, longitudinal approaches. As our understanding of the biology of PTSD grows, we will be able to understand mechanisms of actions of various treatments.
PTSD and Affective Disorders:
The overlap of symptoms between PTSD and depressive disorders is substantial. Key features of both disorders include sleep disturbance, decreased concentration, avoidance and withdrawal, lack of interest and pleasure in activities, and a sense of isolation and distance from others. PTSD with or without major depression, appears to be an important risk factor for suicidality. The presence of suicidal behavior was found to be most frequent in individuals with the primary diagnosis of PTSD compared with all other diagnoses. Interestingly, PTSD patients with comorbid depression reported more suicidal ideation than those non-depressed individuals with PTSD. The diagnostic confusion and symptoms overlap between PTSD and other anxiety disorders is considerable. Physiologic symptoms of increased autonomic arousal, intense psychological distress, Derealization or depersonalization, and fear of losing control are all characteristic of both PTSD and panic disorder. Social phobia, specific phobia, agoraphobia, and PTSD all share avoidance symptoms. Sleep disturbance, difficulty concentrating, and restlessness are common to all anxiety disorders. The comorbidity of PTSD and psychotic disorders is a relatively unexplored area, but probably occurs more commonly than expected. During acute hospitalization for psychotic individuals, treatment interventions focus on the stabilization of psychoses and improvement of cognitive disorganization, often leaving PTSD symptoms unrecognized and treated. Eating disorders pathology can represent a desperate attempt for a traumatized patient to regulate overwhelming affective states and construct a coherent sense of self and meaning within a socio-cultural context preoccupied with thinness and beauty.
PTSD and Substance Use Disorders:
A number of studies have documented the common co-occurrence of PTSD, victimization, and substance use disorders. Three major causal pathways have been hypothesized. The self-medication hypothesis; the relationship between these disorders is that substance users because of their high-risk lifestyles place themselves at risk for exposure to trauma and for that reason are more likely to develop PTSD. Third potential explanation for the high comorbidity is that these individuals have poor coping strategies and/or changes in brain neurochemistry that might enhance susceptibility and worsen the course of PTSD. In conclusion, the relationship between PTSD and substance abuse disorders is complex, but it is likely that in many cases, the substance use disorder may develop as an attempt to self-medicate painful symptoms of PTSD. In any individual case, the relationship between these disorders, both in order of onset and symptom exacerbation and presentation, should be explored to provide individually tailored treatment.
PTSD and Chronic Pelvic Pain:
Chronic pelvic pain, is generally defined as non-cyclic pain of at least 6 months duration, severe enough to require medical care or cause disability and occurring in locations such as pelvis, anterior abdominal wall at or below the umbilicus, lower back, or buttocks. Chronic pelvic pain has been estimated to have a prevalence of 15% among women of reproductive age and accounts for 10% of gynecologic consultations and 40% of diagnostic laparoscopies performed in general hospitals. The association of trauma with poor health may be due in part to development of PTSD resulting from trauma. Many women with chronic pelvic pain fail to respond to treatment, relapse rates are high and chronic pelvic pain patients use a disproportionate amount of health care resources. Given that women with chronic pelvic pain have high rates of trauma and are often treatment refractory, this is an ideal population to examine the effects of trauma and PTSD on health status. The patients with PTSD (similar to major depression are more likely to report their pain as severe, compared with those without PTSD, even when there is no apparent objective medical basis for the difference in pain intensity (8). Therefore, comprehensive treatment strategies will need to target PTSD symptoms and histories of trauma or abuse in women with chronic pelvic pain. Furthermore, a self-rated screening instrument for PTSD can serve as a useful tool for triaging patients with a history of trauma in a gynecology setting so that specific treatment interventions may be developed that will address the effect of trauma in chronic pelvic pain. Comorbid PTSD is associated with poor health and related quality-of-life outcomes in other medically ill patient populations. Early diagnosis of PTSD is critical, because prompt initiation of treatment improves long-term outcome and prevents needless and ongoing suffering.
Psychosocial Interventions -- Cognitive Behavioral Treatment (CBT):
Many victims recover from traumatic experiences without developing significant long-term sequelae. Traditionally as well as contemporary conceptualizations of the psychological effects of trauma and its treatment have postulated that special processing of the traumatic experience needs to take place for recovery to occur. Indeed, the idea that the treatment of traumatized individuals should include some form of exposure to the traumatic event has a long history in psychiatry. PTSD was introduced into the DSM-III as an anxiety disorder nearly 2 decades ago. Two sets of cognitive-behavioral procedures have been commonly employed with this disorder: exposure procedures and anxiety management procedures. Exposure procedures encompass techniques designed to help patients confront feared situations, objects, memories, or images and include systematic desensitization and flooding.
In contemporary exposure treatments, patients are typically encouraged to confront the feared and avoided memories and situations in 2 main ways: imaginable exposure -- in which the patient is instructed to vividly imagine the traumatic event and describe it aloud, along with the thoughts and feelings that occurred during the event and in-vivo exposure. This consists of confrontation with external situations, places or activities that will trigger trauma-related fear and anxiety. The second set of treatments comprises anxiety management procedures. This form of cognitive-behavioral treatment includes a set of skills or tools for managing anxiety such as breathing and relaxation training, positive self-dialogue, cognitive restructuring, social skills training, thought stopping, and role-playing. A commonly used and relatively well-studied anxiety management treatment for PTSD is Meichenbaum's stress inoculation training (SIT), adopted by Vernon and Kilpatrick for use with rape victims (6).
Much progress in developing effective psychosocial treatments for PTSD has been made, many patients do not benefit sufficiently and others either refuse to enter treatment or drop out prematurely. The symptoms experienced by individuals with chronic PTSD sometimes interfere with their readiness to engage in treatment, especially the symptom of avoidance. Successful treatment requires a strong and collaborative relationship between patient and therapist. Factors associated good outcome of exposure and cognitive therapy include perception of treatment as credible, high motivation, high and regular attendance, and absence of ongoing environmental stress. Patients with severe PTSD often have problems trusting other people, including the therapist. Therefore the therapist should make special efforts to offer support and convey empathy and caring, including calling the patient between sessions. Flexibility in scheduling, and rescheduling appointments is often required.
Pharmacotherapy -- Antidepressant Treatment:
The pathophysiology of PTSD is considered to be multifactorial, and treatments have historically been targeted toward regulation of a possible pathophysiologic abnormality or toward relief of specific symptomatology. Recent evidence suggests that the serotonergic system as well as the noradrenergic system may be dysregulated in PTSD, and the efficacy of antidepressants is likely to involve enhancement of one or both of these neurotransmitters.
Tricyclic Antidepressants (TCAs) and Monoamine Oxidase Inhibitors (MAOIs): The oldest medication studies have involved tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) and have suggested modest efficacy for these medications. Desipramine (200 mg/day) was reported to be superior to placebo; amitriptyline (mean dose169 mg/day) was superior to placebo; phenelzine (mean dose 66 mg/day) was not superior to placebo. Both imipramine and phenelzine are superior to placebo, and phenelzine is superior to imipramine for decreasing intrusive PTSD symptoms. A quantitative review of the open and controlled trials of TCAs and MAOIs suggest that the global efficacy of phenelzine (82%) exceed the global efficacy of TCAs (45%), owing in part to the specific MAOI benefit for intrusive symptoms. Reversible inhibitors of monoamine oxidase (RIMAs), such as brofaromine and moclobemide, which are not available in the United States, have also been studied in PTSD. Brofaromine (150 mg/day) was not found to be superior to placebo after 12 weeks in the patients with PTSD. An open trial of 12 weeks of moclobemide (600 mg/day) indicated improvement of PTSD symptoms (7).
Selective Serotonin Reuptake Inhibitors (SSRIs): four open trials of fluoxetine with flexible dosing (20-80 mg/day) over at least 8 weeks have suggested that fluoxetine improves many of the symptoms of PTSD. A pilot study suggests that responders from the trial maintained their improvement better with fluoxetine than placebo after 6 months of double-blind treatment. Small open trials with sertraline have suggested improvement in PTSD symptoms in male veterans, rape victims, and subjects with comorbid alcoholism. A pooled analysis indicates that sertraline is significantly more effective than placebo by week 2 of the trials, and the significance was sustained from week 6 onward. It also indicates superiority of sertraline over placebo in improving several quality of life measures.
Other Antidepressants and Mood Stabilizers: Nefazodone shows promise in reducing PTSD symptoms. A pooled analysis of the 92 subjects in these 6 trials indicated that nefazodone was helpful for the 3 PTSD symptom clusters and that response was associated with younger age, being female, and surviving civilian rather than combat trauma. Small open trials suggest that trazodone and clomipramine improve obsessive intrusion symptoms. Venlafaxine, which has both serotonergic and noradrenergic actions, improve both PTSD and major depression symptoms. Mirtazapine (30-40 mg/day) is reported improvement in the symptoms when used as a single medication after 8 weeks and as adjunctive medication with SSRIs after 4 weeks. Mood stabilizers and antiepileptic medications have also been examined for the treatment of PTSD. Lamotrigine (dose up to 500 mg/day), lithium, carbamazepine and valproate have suggested efficacy for some symptoms of PTSD. Mood stabilizers may be particularly effective as single or adjunctive medications for the anger and explosive behavior common in PTSD. Although future treatments of PTSD should target the several possible etiologic factors in PTSD, the SSRIs and other antidepressants are a promising first-line treatment.
Future approaches to Pharmacotherapy:
The pathophysiology of posttraumatic stress disorder (PTSD) is very complex. At present, we have embarked upon an empirical approach in which pharmacologic research consists of clinical trials with agents, such as antidepressants, anxiolytics, and anticonvulsants, initially developed for different purposes. The approach taken here is theoretical rather empirical, starting with what is known about the unique pathophysiology of PTSD and then predicting the types of pharmacologic agents that might prove effective in the future. Such classes of compounds include corticotrophin-releasing factor antagonists, neuropeptides Y enhancers, antiadrenergic compounds, drugs to down-regulate glucocorticoid receptors, more specific serotonergic agents, agents normalizing opioid function, substance P antagonists, N-methyl-D-aspartate facilitators, and antikindling/antisensitization anticonvulsants.
Summary:
Traumatic exposure and PTSD have an impact on the individual's health, health care service utilization, and general functioning. Such effects provoke a considerable economic burden not only for those persons experiencing trauma and PTSD, but also for the health care system and society as a whole. Currently, routine evaluation for a history of trauma and PTSD often does not occur in primary care settings or in obstetric and gynecologic settings. Many women with histories of trauma and PTSD are not receiving appropriate care for their psychiatric symptoms. Busy primary care physicians need efficient and easy-to-use instruments to help them triage patients who require further evaluation. Furthermore, multiple studies have demonstrated that obstetricians and gynecologists provide more office-based general medical evaluations for women of reproductive age than either family practice physicians or internists and that increasingly, obstetricians and gynecologists have expanded training and expertise in overall women's primary health care.
Editor's Note:
With respect to mental health interventions, The World Health Report 2001, recommends making mental health treatment available within primary and other health-care settings, which require staff training, supervision, and a referral system. The purpose of this brief review is to stimulate new approaches to the pharmacotherapy of PTSD. Given the unique pathophysiology of this disorder, it seems that careful consideration of PTSD-related abnormalities in the human stress response should provide valuable hints for future pharmacotherapy of this disorder.
Resources:
- World Health Organization
List of Guidelines for Health Emergencies -- Posttraumatic Stress Disorder (PTSD) - National Institute of Mental Health -- National Institute of Health (NIH)
Posttraumatic Stress Disorder (PTSD) - Center for Disease Control and Prevention (CDC)
Coping With a Traumatic Event
References:
- Diagnostic and statistical manual of mental disorders. (DSM-IV). 4th ed. Washington DC: American Psychiatric Association; 1994.
- Samson AY, Bensen S, Beck A et al. Post-traumatic stress disorder in primary care. J Fam Pract 1999;48:222-7.
- Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992;60:409-18.
- Davidson JR, Hughes D, Blazer DG et al. Posttraumatic stress disorder in the community: an epidemiological study. Psychol Med 1991;21:713-722.
- Yehuda R. Posttraumatic stress disorder. N Engl J Med 2002;346:108-14.
- Lecrubier Y. Posttraumatic stress disorder in primary care: a hidden diagnosis. J Clin Psychiatry 2004;65 (suppl): 49-54.
- Schoenfeld FB, Marmar CR, Neylan TC. Current concepts in pharmacotherapy for posttraumatic stress disorder. Psychiatr Serv. 2004;55:519-31.
- Meltzer-Brody S, Leserman J, Zolnoun D et al. Trauma and Posttraumatic Stress Disorder in women with chronic pelvic pain. Obstet & Gynecol. 2007;109:902-908.
Published: 20 February 2009
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


