Infertility: Evaluation & Management
WHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC).
An estimated 10% to 15% of couples who want to have a child have difficulty conceiving. At least 6.2 million couples in USA are infertile. Some experts place that number closer to 8 million. It is clear that infertility is an immense problem, not only because of the vast number of people affected, but also because of the heartache they suffer and the costs incurred by the healthcare system. Although the incidence of infertility seems to be on the rise, it is not clear whether this trend represents an actual increase in infertility or just a greater demand for infertility services. However, some social developments appear to have increased the prevalence of factors associated with infertility. Many couples with fertility problems prefer to try to conceive rather than adopt, not only for the obvious emotional reasons but because they fear that adopted babies may have health problems associated with in-utero exposure to human immunodeficiency virus (HIV) or illicit drugs. These factors have placed greater emphasis on the diagnosis and treatment of infertility. Current management treatment plans and exciting research for the future allow ever-increasing optimism for these couples.
The purpose of this document is to provide the understanding of evaluation of infertile couple and strategies for the management of infertility. One of the main challenges before us today is matching the right patient with the right intervention. Fertility decreases with age, especially in women; therefore the common practice of delaying childbearing for a variety of economic and social reasons has probably added to number of couples who are unable to conceive naturally. The incidence of sexually transmitted diseases that can damage reproductive structures in both men and women has risen significantly. Fortunately, we have more resources than ever for investigating the causes of infertility and then treating the condition effectively.
Reproductive Physiology:
Complex hormonal interactions control both development and function of the reproductive tracts in both women and men. The hypothalamic-pituitary-gonadal axis stimulates and regulates the production of the hormones needed for normal sexual development and function. Both the ovary and the testis are controlled through a complex hormonal system with positive and negative feed-back loops. The hypothalamus produces gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland to produce and release two gonadotropic hormones: follicular-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH in turn stimulate the ovary and testis to produce steroid sex hormones like testosterone and estrogen as well as gametes. The sex steroids "feed back" to the hypothalamus and pituitary to regulate the secretion of GnRH, FSH and LH.
Men -- the gonadotropic hormones FSH and LH act on the testes. Both are necessary to initiate spermatogenesis. LH stimulates the Leydig cells of the testes to secrete testosterone, a hormone essential for spermatogenesis and for the development of secondary sex characteristics in men. Testosterone regulates the production of LH. When testosterone reaches a certain level, it exerts a feedback influence on the pituitary and hypothalamus to regulate the production of FSH which is produced by the Sertoli cells or the germ cells of the testes, or both. Each testis consists of several hundred lobules containing coiled seminiferous tubules that converge to form the rete testis. The rete testis in turn empties into the ductuli efferentes testis. It takes about 72 days for an immature spermatogonium to develop into a mature spermatozoon. The sperm formed in the seminiferous tubules mature and attain motility in the epididymis. From the epididymis, the sperms enter the vas deferens, which travels through the scrotum, enters the inguinal canal and courses through the pelvis to the posterior part of prostate. The sperm and accompanying fluids are deposited in the prostatic urethra. The prostate contributes acid-phosphatase and fibrinolysins that break up sperm coagulant. Ejaculation occurs when the seminal fluid reaches the prostatic urethra and is propelled forward by the action of the bulbocavernosus muscle, which is controlled by sympathetic stimulation. Sensory nerves in the prostatic urethra carry afferent impulses to the autonomic nervous system, which stimulates the internal sphincter to contract, preventing retrograde flow into the bladder. Parasympathetic nerves stimulate the external sphincter causing it to relax.
Women -- in women the action of gonadotropic hormones is cyclic. When estrogen levels reach their lowest point, menstruation occurs; at the same time FSH and LH levels are rising gradually. The increasing quantities of gonadotropins stimulate the growth of numerous ovarian follicles, which produce higher levels of estrogen in response to rising levels of LH and FSH. Of the many follicles that begin to mature, only one normally progresses to become a mature follicle; the others degenerate. The mechanism that causes this degeneration and the eventual ascendancy of one follicle is known to occur via apoptosis. It is known, however, that the dominant follicle produces more estrogen, which makes the follicle more susceptible to gonadotropic stimulation. As the cycle progresses, estrogen production increases and the production of gonadotropins (primarily FSH) is somewhat suppressed by a negative estrogen feedback. Estrogen levels continue to rise and eventually exert a biphasic (positive) feedback on the hypothalamic-pituitary system, resulting in a surge of LH and a lesser surge of FSH. An ovum is extruded from the mature follicle 24 to 48 hours later. After ovulation, the empty follicle becomes the corpus luteum, which begins to secrete progesterone and contributes to the production of estrogen. The progressive rise in serum levels of these two hormones transforms the endometrium of the uterus into a secretory lining in preparation for pregnancy. If pregnancy does not occur, the corpus luteum with a life-span of about 14 days, begins to decay. The production of progesterone and estrogen by the corpus luteum begins to decrease, and menstruation begins. When pregnancy does occur, the conceptus secretes, human chorionic gonadotropin (HCG), which maintains the function of the corpus luteum. The corpus luteum continues to produce increasing amounts of progesterone and estrogen for up to 10 weeks. These hormones are essential for maintaining the pregnancy. If the effect of progesterone on the endometrium is inadequate, the pregnancy is lost. Just as fertility decreases with increasing age, the incidence of clinically recognized spontaneous miscarriage rises as age advances (1).
Ovulatory Cycle
General Principles in the Evaluation of Infertility:
The evaluation of infertility should focus on the couple and not on one or the other partner, regardless of past reproductive performance. Both partners should be encouraged to attend each visit during evaluation, whenever possible. Couples undergoing infertility diagnosis and treatment may require counseling for emotional difficulties such as anxiety, stress, and depression. Healthcare providers caring for infertile couples should keep 5 basic goals in mind:
- Identify the specific cause of infertility, when possible and utilize proper evaluation and treatment method.
- To provide accurate information and the options available to the couple. Regular consultations to review and critique results and to outline recommendations for further evaluation and treatment are necessary to ensure that all of the couple's medical, emotional and financial needs and concerns are effectively addressed.
- To guide the couples in whom standard forms of treatment do not achieve success to alternatives, including Assisted Reproductive Technologies (ART), the use of donor gametes (oocytes or sperm).
- To provide emotional support during a trying time. Infertile couples often need the opportunity to express their concerns, frustrations, and fears. Support group or counseling services are beneficial and can help to meet the need. Counseling must be an ongoing process during both evaluation and treatment (2).
- To provide information and refer to adoption services or resources, if desired by the couple and to help them to come to closure.
Clinical Evaluation:
All couples and particularly infertile couples are very interested in learning anything that they themselves might do to maximize the likelihood of achieving a successful pregnancy. With unprotected intercourse, about 90% of normally fertile couples conceive within 1 year (20% within 1 month, 50% within 3 months, and 75% within 9 months). Therefore, most couples should not be subjected to the rigors of an infertility work-up until they have tried to conceive for at least 1 year without success. If a couple seek medical help for fertility problems before 1 year has elapsed, a thorough history and physical examination are warranted to help them decide whether to proceed with further testing. If the history or examination reveals impaired spermatogenesis, apparent menstrual dysfunction, pelvic inflammatory disease, prior pelvic surgery, or obvious sexual dysfunction, there is no reason to wait. The woman's age (>35 years) may also be a reason to initiate fertility evaluation earlier. Some couples elect to wait the full year, while others proceed with non-invasive and less expensive tests.
Lifestyle choices and environmental factors can indeed influence fertility and deserve consideration and discussion when they are relevant. Approximately 62% of American women are overweight and another 33% are obese (3). Abnormalities of hypothalamic GnRH and pituitary gonadotropin secretion are relatively common in overweight (BMI greater than 25), obese (BMI greater than 30) and underweight (BMI less than 17) women. The relationship between BMI and fertility in men has not been carefully studied. One of few things over which the couple can have specific control is any form of substance abuse; smoking is the most important. Smoking has a well-known adverse impact on pregnancy outcome and there is mounting evidence that fertility is lower particularly in women who smoke. The mechanisms involved can include accelerated follicular depletion. Other forms of substance abuse can also adversely affect fertility. Marijuana inhibits the secretion of GnRH and can suppress reproductive function both in men and women. Cocaine use can impair spermatogenesis and has been associated with a markedly increased risk of tubal disease in women. Heavy alcohol consumption in women decreases fertility (4). These lifestyle factors also increase the risk of pregnancy loss.
History and Physical Examination:
Any evaluation of infertility begins with a careful history and physical examination which often will identify symptoms or signs that suggest a specific cause and help to focus evaluation on the factor(s) most likely responsible. Initial interview should document both duration of unprotected intercourse and ages of both partners. Women 35 years and older should be counseled about age-related fertility problems: reduced contraception rate, increased morbidity and/or mortality during pregnancy, and genetic abnormalities in the fetus. Prenatal screening for Down syndrome and other chromosomal abnormalities should be discussed at this time. In the female partner, particularly relevant medical history and physical findings include the following: gravidity, parity, pregnancy outcomes and associated outcomes; menstrual cycle length, characteristics, onset and severity of dysmenorrhea; duration of infertility and results of any previous evaluation and treatment. Nutritional status, marked increase in physical activity, or decrease in weight may signal ovulatory dysfunction. Both partners need to be questioned about previous pelvic surgery because it may be associated with functional impairment of the reproductive tract. With any pelvic surgery, formation of adhesions can block or impair tubal function in women. In men, surgery for inguinal hernia may cause inadvertent vasectomy or interfere with blood supply to the testes. Previous abnormal Pap smear and any subsequent treatment; current medication; allergies; occupation and use of tobacco, alcohol and other illicit drugs are very important part of assessment. Symptoms of thyroid disease, pelvic or abdominal pain, galactorrhea, hirsutism, dyspareunia, family history birth defects, mental retardation, early menopause or reproductive failure should be inquired during history.
Physical examination -- weight and body mass index (BMI), thyroid enlargement, nodule or tenderness, breast secretions and their character, signs of androgen excess -- hair on face, abdomen, arms and leg; pelvic or abdominal tenderness, pelvic mass, vaginal or cervical abnormality, secretions or discharge, tenderness or nodularity in the adnexa or cul-de-sac. Screening for sexually-transmitted infections is recommended for all women at moderate to high risk for infection. The American College of Obstetricians and Gynecologists and the American college of Medical Genetics recommend that screening for cystic fibrosis be made available to all couples seeking preconception or prenatal care (not just those with a personal or family history of cystic fibrosis as previously recommended) and that screening should be specifically offered to couples in ethnic or racial groups considered at higher risk for carrying a cystic fibrosis mutation (Caucasians, particularly those of Ashkenazi Jewish descent) (5). All women who are attempting to conceive in whom previous rubella infection or vaccination cannot be documented should be tested for rubella immunity and vaccinated if seronegative. Recommendations regarding screening for varicella (chicken-pox) immunity are more controversial. Before therapeutic donor insemination and in prospective recipients of donor oocytes or embryos, the American Society for Reproductive Medicine (ASRM) recommends sexually transmitted diseases screening for both partners; for male partners of women to be inseminated, the ASRM also strongly recommends HIV testing. For recipients of donor oocytes or embryos and their male partners, the ASRM recommends screening for syphilis, hepatitis B and C, and HIV.
Diagnostic Procedures:
Before any formal investigation begins, the major causes of infertility and the basic components of the infertility evaluation designed to identify them should be outlined for the couple. The major causes of infertility include ovulatory dysfunction (15%), tubal and peritoneal pathology (30-40%), and male factors (30-40%); uterine pathology is generally uncommon, and rest is largely unexplained. The standard systematic approach to infertility diagnosis involves inexpensive and non-invasive tests first, then proceeds to the more costly or invasive procedures. The tests for infertility can usually be completed within two ovulatory cycles. Typical sequence of infertility work-up:
Step 1 -- Initial interview and examination; tests for sexually transmitted diseases; discuss
findings of history and physical
examination and outline tests, answer questions and concerns to patient and her partner.
Step 2 -- Laboratory evaluations:
Men: Semen analysis (after suitable abstinence)
Women: Basal Body Temperature (BBT);
Ovulation detection kit (beginning on day 10 in women with a 28 day cycle) (6);
Hormone assays as per indication (FSH, TSH, Prolactin, DHEAS);
Hysterosalpingography (HSG) -- can be days 5-13 you want it to be after bleeding has stopped but before
ovulation, if there is no evidence of vaginal or sexually transmitted diseases.
For amenorrhea or severe oligomenorrhea, begin with hormonal studies and after induction of ovulation, proceed
to above studies.
Step 3 -- Laparoscopy and endometrial biopsy:
Hysterosalpingogram shows tubal patency -- laparoscopy (if indicated) during luteal phase
Hysterosalpingogram suggests possible tubal blockage -- laparoscopy (during early follicular phase) and endometrial-
biopsy in late luteal phase in office. (Barrier contraception necessary at this time).
Step 4 -- Continue investigation based on positive findings
The human reproductive process is obviously complex. However, for purposes of evaluation, it can be effectively broken down into its most important and basic component parts. The infertility evaluation is designed to isolate the integrity of each of these components, insofar as that is possible, and to identify any abnormalities that might impair or prevent conception. The pace and extent of evaluation are based on the couple's wishes, age, duration of infertility, and any unique features of the medical history or physical examination.
- Male Factor -- sperm must be deposited at or near the cervix at or near the time of ovulation, ascend into the fallopian tubes, and have the capacity to fertilize the oocyte.
- Ovarian Factor -- ovulation of a mature oocyte must occur, ideally on a regular, predictable, cyclic basis.
- Cervical Factor -- cervix must capture, filter, nurture, and release sperm into the uterus and fallopian tubes.
- Tubal Factor -- fallopian tubes must capture ovulated ova and effectively transport sperm and embryos.
- Uterine Factor -- uterus must be receptive to embryo implantation and capable of supporting subsequent normal growth and development.
Male Factor:
Abnormalities in the male are the sole cause of infertility in approximately 20% of infertile couples and are an important contributing factor in another 20-40% of couples with reproductive failure. Many infertile men have medically or surgically correctable disorders that, if properly diagnosed and treated, can be overcome to allow them to achieve a natural conception with their partners. In others, mild but important semen abnormalities are amenable to intrauterine insemination (IUI). When all else is futile or fails, modern assisted reproductive technologies (ART) can still provide the means to achieve success. In vitro fertilization (IVF) by intracytoplasmic sperm injection (ICSI) involves the injection of a single sperm directly into a mature oocyte offers men heretofore considered hopelessly infertile, a realistic chance to father children. Artificial insemination using donor sperm, once the only option for many couples with male factor infertility, remains an important and highly effective treatment strategy. Although aging has adverse effects on male reproductive function, the impact of age is less obvious than it is in women. Semen quality and male infertility as well as androgen production and serum testosterone levels decrease very gradually as age increases.
The initial evaluation for male factor infertility should include at least 2 properly performed semen analyses obtained at least 4 weeks apart. Semen parameters can vary widely over time, even among fertile men, and also exhibit seasonal variations (6). Overall, the odds of male infertility increase with the number of major semen parameters (concentration, motility, morphology) in the subfertile range; the probability is 2-3 times higher when one is abnormal, 5-7 times higher when two are abnormal and 16 times greater when all three are abnormal. Semen analysis normal reference values are: volume -- 1.5 to 5.0 mL; pH - >7.2; viscosity - <3 (scale 0-4); sperm concentration - >20 million / mL; total sperm number - >40 million / ejaculate; percent motility - >50%; forward progression - >2 (scale 0-4); normal morphology - >50% normal, >30% normal, >14% normal; round cells - <5 million / mL; sperm agglutination - <2 (scale 0-3). Azoospermia describes the absence of sperm on standard microscopic examination. The prevalence of azoospermia is approximately 1% in all men and 10-15% in all men with infertility. Urologic evaluation, if not performed earlier, grossly abnormal semen parameters are indication for a thorough physical examination by an urologist or other specialist in male reproduction; some men also may require further urologic evaluation.
Ovarian Factor: Ovulatory Dysfunction
Cervical Factor:
The cervix and cervical mucus participate in the reproductive process in several ways. Cervical mucus accepts or captures sperm from the ejaculate and the vagina, excludes all other seminal plasma constituents and filters out morphologically abnormal sperm, nurtures sperm biochemically, and serves as a reservoir for sperm, thereby prolonging their survival and the interval between intercourse and ovulation that will allow conception. Cyclical changes in cervical mucus characteristics help to explain why the cycle day-specific probability of conception rises steadily as ovulation nears and plummets immediately thereafter. The reduced secretion of cervical mucus may be caused by a number of factors, including LEEP conization and cauterization of cervix that destroys the mucus-secreting glands of the endocervix. Occasionally, clomiphene therapy suppresses mucus secretion. Estrogen stimulates cervical mucus production and progesterone inhibits it.
The postcoital test -- also known as the Sims-Huhner test has been the traditional method for identifying cervical factor infertility. It has been a part of infertility evaluation for more than 100 years, but the clear consensus of opinion in the U.S. is that its time has passed (8). The test result has little or no value for planning treatment in the large majority of couples. Moreover, scheduled intercourse and office examination soon thereafter are also an inconvenient, embarrassing, and unwelcome intrusion for many couples, adding further to their burden of stress. Therefore, routine postcoital testing is unnecessary. It may be safely reserved for those few in whom results will clearly affect the treatment strategy.
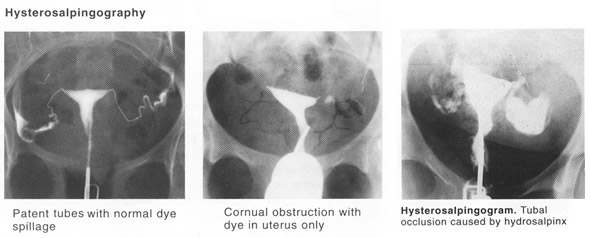
Tubal Factor:
Tubal occlusion and adnexal adhesions are among the most common causes of infertility and the primary diagnosis in approximately 30-35% of infertile couples. A history of pelvic inflammatory disease (PID), septic abortion, ruptured appendix, tubal surgery, or ectopic pregnancy suggests the possibility of tubal damage. PID is unquestionably the major cause of tubal factor infertility and ectopic pregnancies. Classic studies in women with PID diagnosed by laparoscopy have revealed that the risk of subsequent tubal infertility increases with the number and severity of pelvic infections; overall, the incidence is approximately 10-12% after one episode, 23-35% after two, and 54-75% after three episodes of acute PID (9). Hysterosalpingography (HSG) and laparoscopy are the two classic methods for evaluation of tubal patency in infertile women and are complementary rather than mutually exclusive; each provides useful information that the other does not and each has advantages and disadvantages. HSG images the uterine cavity and reveals the internal architecture of the tubal lumen, neither of which can be evaluated by laparoscopy. Laparoscopy provides detailed information about the pelvic anatomy that HSG cannot, including adhesions, endometriosis, and ovarian pathology. HSG is best scheduled during the 2-5 day interval immediately following the end of menses to minimize risk of infection, avoid interference from intrauterine blood and clot, and prevent any possibility that and HSG might be performed in a not yet conception cycle. Debate regarding the relative advantages and disadvantages of oil- and water-soluble contrast media has raged for years. Either media is an appropriate choice. The clinical implications are that when HSG reveals obstruction there is still a relatively high probability (approximately 60%) that the tube is in fact open (secondary to spasm), but when HSG demonstrates patency there is little chance the tube is actually occluded (approximately 5%).
Uterine Factor:
Abnormalities of the uterus are a relatively uncommon cause of infertility but should always be considered. The anatomic uterine abnormalities that may adversely affect fertility include congenital malformations, leiomyomas, and intrauterine adhesions; endometrial polyps have also been implicated, but their reproductive implications are most unclear. There are three basic methods for evaluation of the uterine cavity, including hysterosalpingography (HSG), standard transvaginal ultrasound or transvaginal ultrasound with saline contrast (sonohysterography) and hysteroscopy. Each has advantages and disadvantages and the choice among them should be tailored to the needs of the individual patient.
Unexplained Infertility:
It is diagnosed when all of the standard elements of the infertility evaluation yield normal results. The incidence of unexplained infertility ranges from 10% to as high as 30% among infertile populations. At a minimum, the diagnosis of unexplained infertility implies a normal semen analysis, objective evidence of ovulation, a normal uterine cavity, and bilateral tubal patency. The necessity for diagnostic laparoscopy in the evaluation of couples with unexplained infertility has been controversial. Laparoscopy certainly can reveal otherwise undetected tubal factors and endometriosis that merit specific treatment or that could limit the effectiveness of empirical treatments. Unexplained infertility likely represents either the lower extreme of the normal distribution of reproductive efficiency or abnormalities of sperm or oocyte function, fertilization, implantation, or pre-embryo development that cannot be reliably detected by standard methods of evaluation. The likelihood of a treatment-independent pregnancy decreases progressively with increasing age of the female partner and increasing duration of infertility. After 3 years of infertility, the likelihood of a spontaneous pregnancy falls to approximately 40%, and after 5 years the likelihood of a spontaneous pregnancy falls to 20% of what it was when the couple began efforts to conceive. Although many couples with unexplained infertility may be expected to conceive without treatment, their already low and steadily declining cycle fecundity provides ample justification for offering treatment to those concerned enough to consult a physician.
All treatments for unexplained infertility are empirical and all are designed, one way or another, to increase gamete density, bringing together more than the usual numbers of eggs and sperm in a timely way. Recommended treatments for unexplained infertility have included intrauterine insemination (IUI), ovarian stimulation (clomiphene citrate, exogenous gonadotropins) to achieve super-ovulation of more than a single ovum, super-ovulation combined with IUI, and assisted reproductive technologies (ART). Among couples with unexplained infertility, in-vitro fertilization (IVF) is the preferred treatment for some and the treatment of last resort for others (10). Overall, the treatment effects of the various therapies for unexplained infertility are relatively small, and treatment may only hasten pregnancy for couples who would ultimately conceive on their own, given time.
Legal and Ethical Decision-Making in Reproductive Medicine:
Constant advances in technology and ethical controversy ensure it has a high public profile. In the United States and throughout the world, today's healthcare providers are challenged by the impact of assisted reproductive technology. Although the deliberate creation of human embryos for scientific research is complicated by ethical and practical issues, a detailed understanding of the cellular and molecular events occurring during human fertilization is essential, particularly for understanding infertility. In the United States, there is the need to improve maternal and fetal/neonatal mortality and morbidity by proposing legislation regulating assisted reproductive technology (ART) and supporting single embryo transfers with no more than 2 such transfers (11). Beginning with the diagnosis of infertility, providers have a responsibility to educate, inform, and treat infertile couples. From the moment pregnancy with multiples is confirmed, the families are faced with incredible stressors including decision making on multifetal or selective reduction. Currently in the United States, legislation does not regulate ART, including ovulation induction / enhancement and IVF. Although the United States does have self-regulation via limited reporting through their professional organization and the Center for Disease Control and Prevention, an unlimited number of embryos may be transferred. Unfortunately, many healthcare providers have not recognized the responsibility and burden placed on families and society as a whole. Lack of regulation means women may become pregnant with high order multiples, which raises serious moral and ethical issues.
Great strides have been made in assisted reproductive technology (ART) and nearly all forms of subfertility are now amenable to treatment. The concept of "when life begins" is much more nuanced to most Americans (12). With a fundamental belief that all life is sacred and begins at conception -- a single cell zygote has the potential to become a person. This is the moral logic. American public continues to support the policies involved and we hope this chapter sets out the basis on which the judgments are made. At the dawn of the genomic era, with its unprecedented research, there is an opportunity to ask the right questions.
Summary:
The physician and patients must decide, using statistical guidelines, when more aggressive and invasive measures should be considered or when treatment should be stopped. Because diagnosis and treatment of infertility can be financially taxing and stressful for some couples, physicians may opt to stop treatment before exhausting all possibilities. Stopping all diagnostic and therapeutic maneuvers for a few months may provide the couple with the mental and physical rest needed to proceed with a complete investigation and treatment. In some couples, even though the infertility has been totally resistant to aggressive treatment, the woman conceives spontaneously while waiting to start in vitro fertilization or after discontinuing treatment.
When all options have been exhausted or the couple no longer wish to continue treatment, adoption should be discussed and resources provided. However, since requests for adoption far outnumber the available adoptable healthy babies, this must be discussed openly with the couple. Counseling can help couples cope with the possibility of remaining childless.
I. Understanding Assisted Reproductive Technology (ART)
II. Psychological Impact of Infertility
III. Ethical Issues in Reproductive Health: That Delicate Balance
Acknowledgement: Gratitude is expressed to Dr. Bradley J. Van Voorhis for sharing his expertise and research to this symposium. We at Women's Health and Education Center (WHEC) are grateful to him for his friendship, support and guidance. His insights in reproductive endocrinology have influenced a great deal in preparing this manuscript.
References:
- Nikolaou D, Templeton A. Early ovarian aging: a hypothesis -- Detection and clinical relevance. Hum Reprod. 2003;18:1137-1140
- Chen TH, Chang SP, Tsai CF et al. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19(10)2313-2318
- National Institute of Diabetes & Digestive & Kidney Disease of the NIH. Statistics related to overweight and obesity. niddk.nih.gov/health/nutrit/pubs/statobes.htm. Accessed February 10, 2006
- Hull MG, North K, Taylor H et al. Delayed conception and active and passive smoking. The Avon Longitudinal Study of Pregnancy and Childhood Study Team. Fertil Steril. 2000;74:725-730
- American Society for Reproductive Medicine. Optimal evaluation of the infertile female. A practice committee report, Birmingham, AL, 2000
- Nielsen MS, Barton SD, Hatasaka HH et al. Comparison of several one-step home urinary luteinizing hormone detection test kits to OvuQuick. Fertil Steril. 2001;76:384-387
- Chen Z, Toth T, Godfrey-Bailey L et al. Seasonal variation and age-related changes in human semen parameters. J Androl. 2003;24:226-229
- Oei SG, Keirse MJ, Bloemenkamp KW et al. European postcoital tests: opinions and practice. Br J Obstet Gynaecol. 1995;102-106
- Evers JLH, Land JA, Mol BW. Evidence-based medicine for diagnostic question. Seminars Reprod Med. 2003;21:9-15
- Goverde AJ, McDonnell J, Vermeiden JP et al. Intrauterine insemination or in-vitro fertilization in idiopathic subfertility and male subfertility: a randomized trial and cost-effectiveness analysis. Lancet. 2000;13:355-360
- Licciardi F, Berkeley AS, Krey L et al. A two- versus three-embryo transfer: the oocyte donation model. Fertil Steril. 2001;75:510-513
- Sandel MJ. Embryo ethics -- the moral logic of stem-cell research. N Engl J Med. 2004;351:207-209
Published: 23 September 2009
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


